Baby sleep disorders symptoms can silently rob your infant of healthy development while you remain unaware that something serious is wrong. Sleep represents far more than rest for your baby, it’s the critical foundation upon which their entire developmental future is built. During those precious hours of slumber, your infant’s brain processes experiences, consolidates memories, releases growth hormones, and undergoes the complex neural development that will determine their cognitive abilities, emotional regulation, and physical health for life. Yet terrifyingly, serious infant sleep disorders can devastate this essential development, creating consequences that may not become apparent until irreversible damage has already occurred.
The heartbreaking reality is that many baby sleep problems go unrecognized for months or even years, while precious developmental windows close and opportunities for optimal growth slip away forever. Unlike older children who can verbalize their sleep difficulties, babies depend entirely on their parents to recognize the infant sleep apnea warning signs and other critical symptoms that their sleep is being disrupted by dangerous conditions requiring immediate medical intervention.
This essential guide will transform you from an exhausted parent struggling with sleepless nights into a knowledgeable guardian capable of recognizing when your baby’s sleep problems signal serious medical conditions that demand immediate professional attention.
Understanding Critical Baby Sleep Disorders Symptoms in Infancy
Sleep serves as the master regulator of infant development, orchestrating complex processes that shape your baby’s future capabilities. During deep sleep, babies’ brains experience rapid eye movement (REM) periods that are crucial for memory consolidation, neural pathway formation, and cognitive development. The American Academy of Sleep Medicine emphasizes that disrupted sleep during infancy can permanently affect brain architecture, leading to learning disabilities, behavioral problems, and developmental delays that persist throughout life.
Newborns require 14-17 hours of sleep daily, with this requirement gradually decreasing as they mature. However, it’s not just the quantity of sleep that matters, the quality and continuity of sleep cycles are equally critical for proper development. Fragmented or disrupted sleep prevents babies from completing essential developmental processes, creating cumulative deficits that compound over time.
Additionally, sleep disorders can interfere with growth hormone release, which primarily occurs during deep sleep stages. This disruption can lead to failure to thrive, delayed physical development, and compromised immune function that leaves babies vulnerable to frequent illnesses and infections.
The American Academy of Sleep Medicine emphasizes that disrupted sleep during infancy can permanently affect brain architecture.
Infant Sleep Apnea Warning Signs: The Silent Suffocation Threat
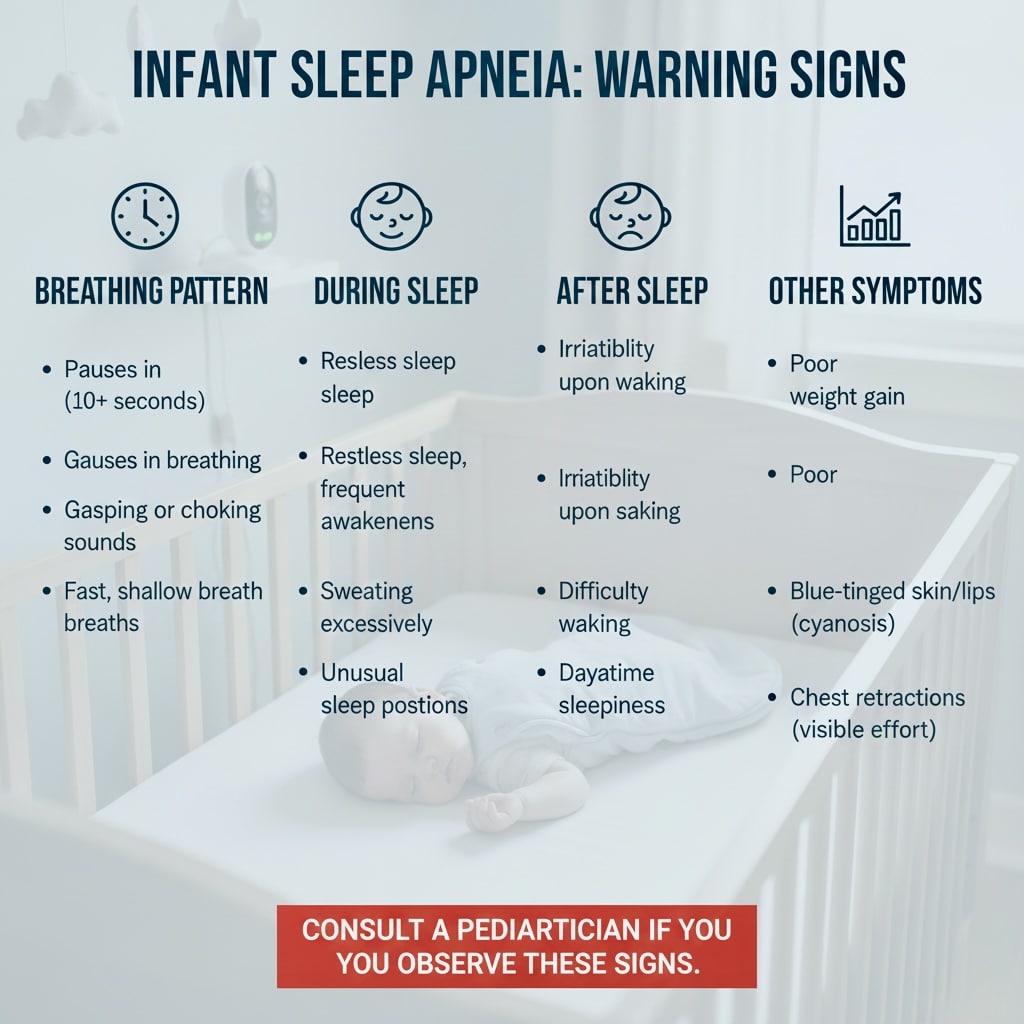
Infant sleep apnea warning signs represent one of the most dangerous baby sleep disorders symptoms, causing babies to repeatedly stop breathing during sleep, leading to oxygen deprivation that can cause brain damage, developmental delays, and death. Unlike adult sleep apnea, infant sleep apnea often occurs without obvious symptoms, making recognition particularly challenging for parents.
Central Sleep Apnea: This condition occurs when the brain fails to send proper signals to breathing muscles, causing breathing to stop completely for periods of 20 seconds or longer. Central sleep apnea is more common in premature babies whose respiratory control centers are still immature, but it can also affect full-term infants.
Obstructive Sleep Apnea: While less common in young infants, obstructive sleep apnea occurs when airways become blocked during sleep, preventing adequate airflow despite continued breathing efforts. This condition can result from enlarged tonsils, unusual facial structure, or other anatomical factors.
Recognition Challenges: Parents may notice pauses in breathing, color changes (blue or pale skin), gasping or choking sounds, excessive sweating during sleep, or unusual sleeping positions where babies arch their necks or sleep with their heads hyperextended. However, many cases of infant sleep apnea produce subtle symptoms that are easily overlooked.
Developmental Consequences: Chronic oxygen deprivation from untreated sleep apnea can cause permanent brain damage, affecting cognitive development, learning abilities, and behavioral regulation. The condition can also strain the cardiovascular system, leading to heart problems and failure to thrive.
How Baby Sleep Disorders Symptoms Impact Development: Timeline
| Age Range | Normal Sleep Development | Impact of Untreated Infant Sleep Disorders |
|---|---|---|
| 0-3 Months | Brain doubles in size, neural pathways form, circadian rhythm develops | Disrupted brain architecture, delayed circadian regulation, growth hormone deficiency |
| 4-6 Months | Memory consolidation improves, sleep cycles mature, motor skills develop | Memory formation problems, motor delays, increased SIDS risk without proper SIDS prevention strategies |
| 7-12 Months | Language processing during sleep, emotional regulation develops, immune system strengthens | Language delays, emotional dysregulation, frequent illnesses, cognitive deficits |
| Long-term (1+ Years) | Foundation for learning, attention, behavior, and physical health established | Learning disabilities, ADHD symptoms, behavioral problems, chronic health issues |
This table illustrates why early recognition of baby sleep disorders symptoms is critical for preventing permanent developmental damage.
Baby Sleep Disorders Symptoms: Quick Reference Guide
| Sleep Disorder | Key Baby Sleep Disorders Symptoms | Age Most Common | Urgency Level |
|---|---|---|---|
| Central Sleep Apnea | Breathing pauses 20+ seconds, blue/pale skin, gasping | 0-6 months (preemies) | 🔴 EMERGENCY |
| Obstructive Sleep Apnea | Snoring, restless sleep, mouth breathing, sweating | 6+ months | 🟡 Urgent |
| SIDS Risk Factors | Stomach sleeping, soft bedding, overheating, smoke exposure | 2-4 months peak | 🔴 EMERGENCY |
| Sleep Fragmentation | Frequent waking (10+ times/night), difficulty settling | 0-12 months | 🟢 Monitor |
| Reflux (GERD) | Arching back, crying during/after feeds, sleep refusal | 0-6 months | 🟡 Urgent |
| Food Allergies | Eczema, digestive issues, restless sleep, irritability | 4+ months | 🟢 Monitor |
Sudden Infant Death Syndrome: SIDS Prevention Strategies: The Unexplained Tragedy
SIDS prevention strategies are essential because Sudden Infant Death Syndrome represents every parent’s worst nightmare, the sudden, unexplained death of an apparently healthy baby during sleep. While the exact mechanisms remain unclear, research suggests that SIDS may involve underlying vulnerabilities in brainstem functions that control breathing, heart rate, and arousal during sleep.
According to the CDC’s SIDS and SUID prevention guidelines, safe sleep practices have reduced SIDS deaths by over 50% since the 1990s.
Essential SIDS Prevention Strategies Checklist
Use this evidence-based checklist to ensure you’re implementing all critical SIDS prevention strategies:
Sleep Position & Environment:
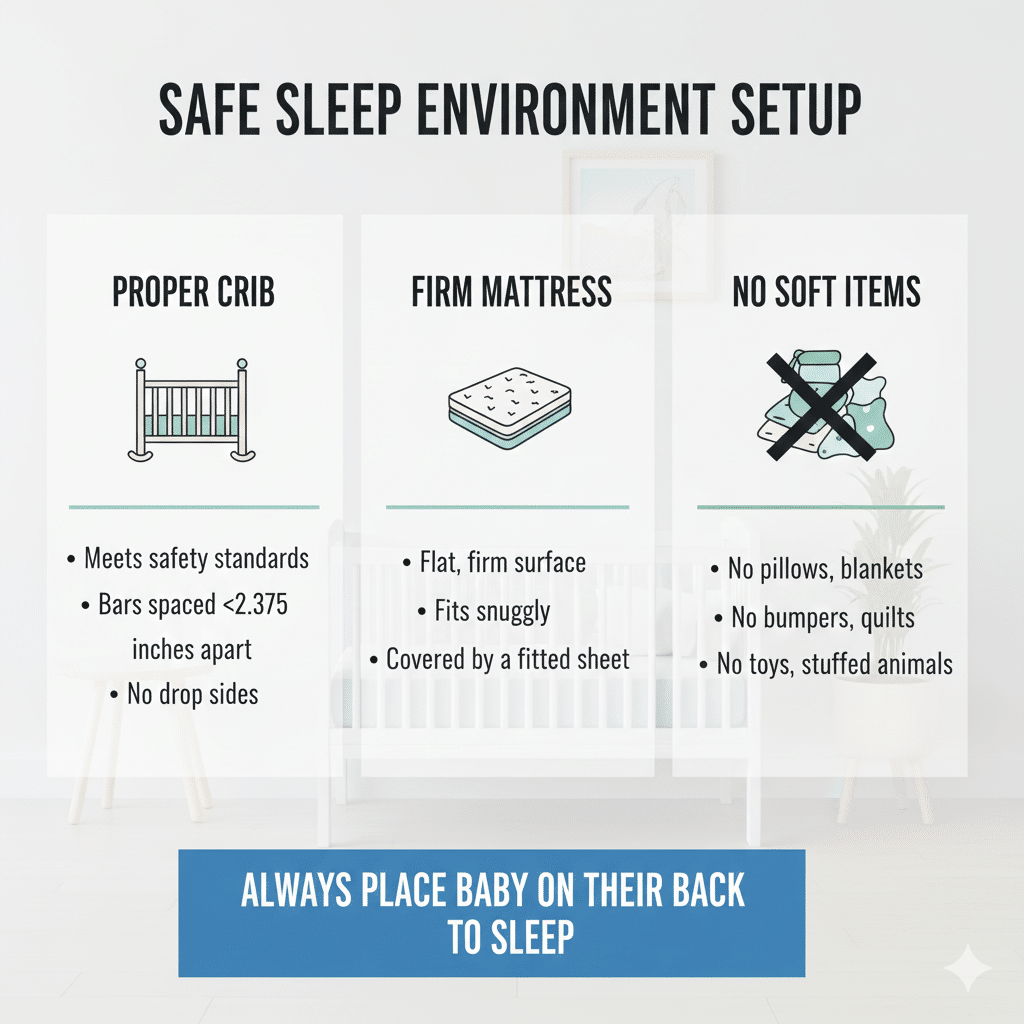
- ✅ Always place baby on back for every sleep (naps and nighttime)
- ✅ Use firm, flat sleep surface (safety-approved crib mattress)
- ✅ Keep crib completely empty (no blankets, pillows, bumpers, or toys)
- ✅ Dress baby in sleep sack instead of loose blankets
- ✅ Maintain room temperature between 68-72°F (20-22°C)
Feeding & Comfort:
- ✅ Breastfeed if possible (provides protective antibodies)
- ✅ Offer pacifier at sleep time (after breastfeeding is established)
- ✅ Never prop bottles or allow baby to sleep while feeding
Room Setup:
- ✅ Room-share (baby in your room) for first 6-12 months
- ✅ Never bed-share (keep baby in separate sleep surface)
- ✅ Remove all soft objects from sleep area
- ✅ Ensure crib meets current safety standards
Smoke & Substance Exposure:
- ✅ Maintain completely smoke-free environment
- ✅ Avoid alcohol and drug use during pregnancy and after birth
- ✅ Keep baby away from secondhand smoke exposure
Medical Care:
- ✅ Attend all well-baby checkups
- ✅ Keep baby up-to-date on immunizations
- ✅ Report any infant sleep apnea warning signs immediately
- ✅ Discuss any concerning baby sleep disorders symptoms with pediatrician
Monitor for Warning Signs:
- ✅ Watch for breathing pauses or color changes during sleep
- ✅ Note any unusual sleeping positions or excessive sweating
- ✅ Document patterns of baby sleep disorders symptoms
- ✅ Trust your instincts and seek help when concerned
Print this checklist and review it regularly to ensure you’re protecting your baby with proven SIDS prevention strategies.
Risk Factor Identification
SIDS risk is highest between 2 to 4 months of age, with 90% of cases occurring before 6 months. Risk factors include premature birth, low birth weight, exposure to smoke during pregnancy or after birth, overheating, soft bedding, and sleeping on stomach or side positions.
The Triple Risk Model: Current SIDS research suggests a “triple risk” model involving a vulnerable infant, a critical developmental period, and external stressors that combine to trigger the fatal event. Understanding this model helps identify babies at higher risk and implement protective strategies.
Evidence-Based SIDS Prevention Strategies
The “Back to Sleep” campaign has dramatically reduced SIDS rates by promoting supine (back) sleeping. Additional protective factors include breastfeeding, using pacifiers at sleep time after breastfeeding is established, avoiding smoke exposure, and maintaining appropriate room temperature.
Creating Safe Sleep Environments: Safe sleep involves using firm sleep surfaces, fitted sheets, and keeping cribs free from blankets, bumpers, toys, and other soft objects. Room-sharing without bed-sharing is recommended for the first 6 to 12 months of life as part of comprehensive SIDS prevention strategies.
Creating a safe sleep environment involves using firm sleep surfaces and the right equipment. Check our comprehensive baby gear guide for recommendations on safe sleep monitors and nursery essentials.
Infant Sleep Disorders and Chronic Sleep Fragmentation
While often dismissed as normal newborn behavior, chronic sleep fragmentation and infant sleep disorders can severely impact development when they persist beyond the expected adjustment period or occur with unusual severity.
Behavioral Insomnia in Babies: This condition involves persistent difficulty falling asleep or staying asleep that isn’t explained by medical conditions. Babies with behavioral insomnia may resist sleep, require extensive parental intervention to fall asleep, and wake frequently throughout the night, showing clear baby sleep disorders symptoms.
Sleep-Onset Association Disorder: Babies develop dependencies on specific conditions or actions to fall asleep, such as being rocked, fed, or held. While some sleep associations are normal, problematic associations prevent babies from developing independent sleep skills and can lead to severely fragmented sleep for the entire family.
Sleep Schedule Disorders: Some babies develop irregular sleep-wake patterns that don’t align with normal circadian rhythms. These disorders can result from neurological immaturity, environmental factors, or underlying medical conditions that disrupt natural sleep regulation.
Developmental Impact: Chronic sleep fragmentation interferes with memory consolidation, emotional regulation, and cognitive development. Babies who don’t achieve adequate consolidated sleep may show delayed language development, poor attention regulation, and increased irritability that affects bonding and social development.

Baby Sleep Problems Related to Medical Conditions
Numerous medical conditions can severely disrupt infant sleep, creating cascading effects on development and family functioning that manifest as persistent baby sleep disorders symptoms.
Central Sleep Apnea in Infants
This condition occurs when the brain fails to send proper signals to breathing muscles, causing breathing to stop completely for periods of 20 seconds or longer. Central sleep apnea is more common in premature babies whose respiratory control centers are still immature, but it can also affect full-term infants.
Research from the National Institutes of Health shows that untreated sleep apnea in infants can lead to serious developmental consequences.
Obstructive Sleep Apnea Recognition
While less common in young infants, obstructive sleep apnea occurs when airways become blocked during sleep, preventing adequate airflow despite continued breathing efforts. This condition can result from enlarged tonsils, unusual facial structure, or other anatomical factors.
Critical Infant Sleep Apnea Warning Signs
Parents may notice pauses in breathing, color changes like blue or pale skin, gasping or choking sounds, excessive sweating during sleep, or unusual sleeping positions where babies arch their necks or sleep with their heads hyperextended. However, many cases of infant sleep apnea produce subtle baby sleep disorders symptoms that are easily overlooked.
Parasomnias and Abnormal Sleep Behaviors
While parasomnias are more common in older children, some abnormal sleep behaviors can occur in infants and may signal underlying neurological or developmental concerns.
Sleep Myoclonus: Benign neonatal sleep myoclonus involves rhythmic jerking movements that occur only during sleep and stop when babies are awakened. While usually harmless, these movements can be mistaken for seizures and require medical evaluation to distinguish between normal and pathological conditions.
Rhythmic Movement Disorders: Some babies engage in repetitive movements like head banging, body rocking, or rolling during sleep transitions. While often normal, excessive or persistent rhythmic movements may indicate developmental delays or neurological conditions requiring evaluation.
Night Terrors in Infants: Though rare in very young babies, night terrors can occur, causing episodes of intense crying, apparent fear, and autonomic arousal during deep sleep stages. These episodes differ from nightmares and may indicate underlying sleep architecture abnormalities.
Confusional Arousals: Some babies experience periods of partial awakening where they appear conscious but confused, crying inconsolably without responding to comfort measures. These episodes may signal immature sleep regulation systems or underlying medical conditions.
Medical Conditions That Disrupt Infant Sleep
Numerous medical conditions can severely disrupt infant sleep, creating cascading effects on development and family functioning.
Gastroesophageal Reflux Disease (GERD): Severe reflux can cause significant sleep disruption as babies wake frequently due to pain and discomfort from stomach acid entering the esophagus. The horizontal sleeping position can worsen symptoms, creating a cycle of poor sleep and worsening reflux.
Food Allergies and Sleep Disruption: Undiagnosed food allergies can cause gastrointestinal discomfort, skin irritation, and systemic inflammation that severely disrupts sleep. Milk protein allergies are particularly common and can cause chronic sleep fragmentation in both formula-fed and breastfed babies.
Respiratory Conditions: Conditions like bronchiolitis, asthma, or chronic lung disease can interfere with comfortable breathing during sleep, causing frequent awakenings and poor sleep quality. These conditions may also increase the risk of sleep apnea and other breathing disorders.
Neurological Conditions: Seizure disorders, brain injuries, or developmental abnormalities can severely disrupt normal sleep architecture, preventing babies from achieving the deep sleep stages essential for development.
Proper nutrition plays a crucial role in sleep quality and overall development. Learn about healthy foods for babies that support better sleep patterns and optimal growth.
Environmental and Lifestyle Factors Affecting Sleep
External factors can significantly impact infant sleep quality and development, often in ways that parents don’t immediately recognize.
Overstimulation: Modern environments often provide excessive sensory input that can overstimulate developing nervous systems, making it difficult for babies to transition to sleep and maintain restful sleep throughout the night.
Schedule Disruptions: Irregular feeding schedules, frequent travel, or inconsistent caregiving routines can disrupt developing circadian rhythms, leading to chronic sleep difficulties that affect development.
Medication Effects: Some medications, including those used to treat common infant conditions, can interfere with normal sleep patterns and architecture, potentially affecting development if not properly managed.
Family Stress: High levels of family stress, maternal depression, or chaotic home environments can affect infant sleep through multiple pathways, including increased cortisol levels and disrupted caregiving routines.
Technology and Sleep Monitoring Solutions
Modern technology offers unprecedented opportunities to monitor infant sleep and identify potential problems before they cause significant developmental impact.

Home Sleep Monitoring: Advanced baby monitors can track breathing patterns, heart rate, and sleep movements, alerting parents to potential problems. However, these devices should supplement, not replace, professional medical evaluation for sleep concerns.
Sleep Study Technology: When serious sleep disorders are suspected, overnight sleep studies (polysomnography) can provide detailed information about sleep architecture, breathing patterns, and neurological function during sleep.
Mobile Applications: Sleep tracking apps designed for infants can help parents identify patterns and potential problems, though they should be used as tools to facilitate communication with healthcare providers rather than for self-diagnosis.
Modern technology offers unprecedented opportunities to monitor infant sleep and identify potential problems before they cause significant developmental impact. The best baby sleep monitoring apps can track breathing patterns, heart rate, and sleep movements, alerting parents to potential problems.
When to Seek Professional Sleep Medicine Evaluation
Emergency Medical Attention for Baby Sleep Disorders Symptoms: Seek emergency care for any episodes where babies stop breathing for more than 20 seconds, turn blue or pale during sleep, or require stimulation to resume breathing. These symptoms suggest serious sleep-related breathing disorders requiring immediate intervention.
Urgent Pediatric Consultation: Contact your pediatrician promptly for persistent difficulty sleeping beyond the newborn period, excessive daytime sleepiness, unusual sleeping positions, or sleep patterns that seem dramatically different from typical infant patterns.
Sleep Medicine Referral: Consider specialized sleep medicine evaluation for babies with chronic sleep difficulties, suspected sleep apnea, or sleep problems associated with developmental delays or medical conditions.
The American Academy of Pediatrics provides comprehensive guidelines for recognizing when sleep problems require professional evaluation.
Building Healthy Sleep Foundations for Optimal Development
Consistency and Routine: Establishing consistent bedtime routines helps regulate developing circadian rhythms and promotes healthy sleep habits that support optimal development while minimizing baby sleep problems.
Environmental Optimization: Creating sleep environments that promote safety and comfort while minimizing stimulation helps babies achieve the deep, restorative sleep essential for development, reducing baby sleep disorders symptoms.
Your vigilance in monitoring your baby’s sleep quality and recognizing potential baby sleep disorders symptoms can prevent minor issues from becoming major developmental obstacles. Trust your instincts, document concerning patterns, and don’t hesitate to seek professional evaluation when your baby’s sleep seems problematic.
Professional Partnership: Working closely with pediatricians and sleep specialists ensures that sleep concerns are addressed promptly before they impact development.
Family Support: Recognizing that healthy infant sleep affects the entire family and seeking support when needed helps maintain the consistency and patience required for addressing sleep challenges.
Your vigilance in monitoring your baby’s sleep quality and recognizing potential problems can prevent minor issues from becoming major developmental obstacles. Trust your instincts, document concerning patterns, and don’t hesitate to seek professional evaluation when your baby’s sleep seems problematic. The investment in ensuring healthy sleep during infancy pays dividends in optimal development, learning capacity, and lifelong well-being for your precious child.
Having the right tools makes managing infant sleep challenges significantly easier. Our guide to essential baby items includes critical sleep safety products every parent needs.
Read more: 7 Essential Baby Sleep Disorders Symptoms Every Parent Must KnowLooking for comprehensive guidance on caring for your baby? Our book ‘How to Care for Children: From Birth to Age 2’ combines professional nanny experience with evidence based child development research. Written by Kelly and Peter, this guide provides clear, reliable advice rooted in real world childcare. Available in English, Spanish, and Portuguese on Amazon.
Click the link below your preferred language to get your copy!

Frequently Asked Questions About Symptoms of Sleep Disorders in Babies
1. What are the most serious baby sleep disorders symptoms I should never ignore?
The most critical baby sleep disorders symptoms requiring immediate emergency care include breathing pauses lasting more than 20 seconds, blue or pale skin color during sleep, requiring stimulation to resume breathing, and choking or gasping sounds. These infant sleep apnea warning signs can indicate life-threatening conditions that need instant medical intervention. Any baby who stops breathing during sleep requires immediate evaluation, as this could signal central sleep apnea or other dangerous respiratory disorders.
2. How can I tell the difference between normal baby sleep problems and serious infant sleep disorders?
Normal baby sleep problems include occasional night wakings, difficulty settling in new environments, and sleep disruptions during developmental leaps or teething. However, serious infant sleep disorders show persistent patterns like chronic breathing pauses, extreme difficulty breathing during sleep, consistent failure to wake for feedings, excessive sweating during sleep, or unusual sleeping positions like extreme neck arching. If baby sleep disorders symptoms persist for more than two weeks despite environmental changes, or if you notice any infant sleep apnea warning signs, seek professional evaluation immediately.
3. At what age are babies most at risk for SIDS and what are the best SIDS prevention strategies?
SIDS risk peaks between 2 to 4 months of age, with 90% of cases occurring before 6 months. The most effective SIDS prevention strategies include always placing babies on their backs to sleep on firm surfaces, keeping cribs free from soft bedding and toys, maintaining comfortable room temperature (68-72°F), avoiding smoke exposure, breastfeeding when possible, and using pacifiers at sleep time after breastfeeding is established. Room-sharing without bed-sharing for the first 6 to 12 months provides additional protection. These evidence-based SIDS prevention strategies have reduced SIDS deaths by over 50% since the 1990s.
4. What infant sleep apnea warning signs should prompt me to call 911 versus schedule a doctor appointment?
Call 911 immediately if your baby stops breathing for more than 20 seconds, turns blue or pale during sleep, becomes limp or unresponsive, or requires vigorous stimulation to resume breathing. These are emergency infant sleep apnea warning signs. Schedule an urgent same-day appointment for concerning patterns like frequent breathing pauses under 20 seconds, persistent snoring in babies under 6 months, extreme difficulty breathing during sleep, or dramatic position changes to improve breathing. Regular appointments are appropriate for mild baby sleep problems like difficulty settling or frequent night wakings without breathing concerns.
5. Can baby sleep disorders symptoms cause permanent developmental damage?
Yes, untreated infant sleep disorders can cause serious, permanent developmental consequences. Chronic oxygen deprivation from sleep apnea can damage developing brain tissue, leading to cognitive delays, learning disabilities, and behavioral problems. Severe sleep fragmentation prevents essential memory consolidation and neural pathway formation during critical developmental windows. Growth hormone disruption from poor sleep quality can cause failure to thrive and delayed physical development. However, early recognition of baby sleep disorders symptoms and prompt treatment can prevent most long-term damage, which is why vigilant monitoring and quick action are crucial for protecting your baby’s developmental future.
6. How do medical conditions like GERD create baby sleep disorders symptoms?
Gastroesophageal reflux disease (GERD) causes stomach acid to flow back into the esophagus, creating intense pain that wakes babies frequently throughout the night. The horizontal sleeping position worsens reflux symptoms, creating a vicious cycle where babies need to sleep but can’t due to pain. This creates characteristic baby sleep disorders symptoms including back arching during sleep, crying immediately after lying down, refusal to sleep flat, and frequent wakings with apparent discomfort. GERD can also increase the risk of aspiration and respiratory problems, potentially contributing to infant sleep apnea warning signs if stomach contents enter the airway during sleep.
7. What role does sleep monitoring technology play in detecting infant sleep disorders?
Modern sleep monitoring technology can detect subtle baby sleep disorders symptoms that parents might miss during nighttime sleep. Advanced monitors track breathing patterns, heart rate, oxygen levels, and movement, alerting parents to potential problems like breathing pauses or irregular heart rhythms. However, technology should supplement, not replace, parental vigilance and professional medical evaluation. False alarms can create anxiety, while over-reliance on monitors might cause parents to miss other important infant sleep apnea warning signs. Use monitoring devices as tools to facilitate early detection and communication with healthcare providers, but always trust your parental instincts when something seems wrong.
8. When should I request a referral to a pediatric sleep specialist for baby sleep problems?
Request a pediatric sleep specialist referral if your baby shows persistent infant sleep apnea warning signs, has been diagnosed with a medical condition affecting sleep (like severe GERD or neurological disorders), experiences chronic sleep fragmentation despite addressing environmental factors, or shows developmental delays potentially related to poor sleep quality. Specialists can perform overnight sleep studies (polysomnography) to diagnose complex infant sleep disorders, identify subtle baby sleep disorders symptoms that standard exams might miss, and create comprehensive treatment plans. Early specialist involvement prevents minor baby sleep problems from escalating into serious developmental obstacles.
Want a complete baby care guide?
Get our FREE checklist sent directly to your inbox - covering everything from birth to age 2, including daily routines, safety guidelines, and developmental milestones.
- ✅ Birth to 3 months essentials
- ✅ 4-12 months routines & alerts
- ✅ 1-2 years development & safety
Enter your email to receive instant access to the PDF