Every parent needs to recognize the warning signs of serious baby digestive problems before they become life-threatening emergencies. This comprehensive guide reveals the 7 most dangerous infant digestive health conditions, including GERD in babies, pyloric stenosis, and critical baby stomach issues that require immediate medical attention. Learn how to protect your child from devastating complications.
Your baby’s digestive system represents both a marvel of rapid development and a source of potentially devastating vulnerabilities that can escalate from minor discomfort to life-threatening emergencies within hours. As a parent, few things feel more helpless than watching your precious infant struggle with feeding difficulties, painful stomach distress, or mysterious digestive symptoms that leave you frantically searching for answers while your baby suffers.
The terrifying reality is that babies’ immature digestive systems make them extraordinarily susceptible to conditions that can cause severe dehydration, malnutrition, and systemic complications requiring immediate medical intervention. Unlike older children who can communicate their discomfort clearly, babies rely entirely on their parents to recognize subtle signs of serious digestive problems before they progress beyond the point of successful treatment.
This essential guide will transform you from an anxious parent into a knowledgeable guardian of your baby’s digestive health, equipped with the expertise to prevent dangerous complications and recognize when immediate medical care becomes critical for your child’s survival.
Building Healthy Family Routines With Your Newborn
Understanding Baby Digestive Problems: What Every Parent Must Know
How Infant Digestive Health Develops in the First Year?
The infant digestive system undergoes dramatic changes during the first year of life, transitioning from the sterile environment of the womb to processing complex nutrients while developing crucial gut bacteria. This developmental process creates windows of vulnerability where seemingly minor issues can quickly become serious health threats.
Newborns are born with immature intestinal barriers, limited digestive enzyme production, and sterile gut environments that must be populated with beneficial bacteria. The American Academy of Pediatrics emphasizes that these developmental factors make babies particularly susceptible to digestive infections, food intolerances, and absorption problems that can rapidly compromise their health.
Additionally, babies’ small stomach capacity and rapid growth requirements mean they need frequent feeding, making any disruption to normal digestive function potentially dangerous for maintaining adequate nutrition and hydration.
The Crucial First Year of Digestive Development
During the first twelve months, your baby’s digestive system undergoes remarkable transformations that establish lifelong health patterns. The gastrointestinal tract develops rapidly, with the stomach capacity increasing from just 20 milliliters at birth to approximately 200 milliliters by six months of age. This rapid expansion requires careful attention to feeding schedules and portion sizes to prevent overwhelming your infant’s developing system.
The protective gut lining strengthens gradually throughout infancy, making newborns particularly vulnerable to infections and inflammatory conditions during the early weeks. Understanding these developmental stages helps parents recognize when digestive symptoms represent normal growing pains versus dangerous medical emergencies requiring immediate intervention.
1. GERD in Babies: When Reflux Becomes Life-Threatening
While most babies experience normal spitting up due to immature lower esophageal sphincles, severe gastroesophageal reflux disease can cause serious complications including failure to thrive, respiratory problems, and esophageal damage.
Recognizing Dangerous GERD: Warning signs include projectile vomiting, blood in vomit or stool, severe crying during or after feeds, arching back during feeding, chronic cough or wheezing, and poor weight gain despite adequate caloric intake. These symptoms indicate reflux severe enough to require immediate medical evaluation.
Complications and Risks: Severe GERD can cause aspiration pneumonia when stomach contents enter the lungs, esophagitis from acid damage, and failure to thrive from inadequate nutrition absorption. Premature babies face particularly high risks due to their underdeveloped digestive systems.
Management Strategies: Positioning babies upright for 30 minutes after feeding, using smaller more frequent meals, and thickening formula (only under medical supervision) can help manage mild reflux. Severe cases may require prescription medications or surgical intervention.

Long-Term Implications of Untreated GERD
When severe reflux remains unmanaged, the consequences extend far beyond immediate discomfort. Chronic acid exposure can damage the esophageal lining, creating scarring that leads to feeding difficulties persisting into childhood. Some babies develop food aversions because they associate eating with pain, creating nutritional challenges that complicate healthy development.
Research demonstrates that babies with poorly controlled reflux show increased risks for respiratory infections due to aspiration events. The constant presence of stomach acid in the esophagus and throat creates inflammation that makes airways more susceptible to bacterial and viral infections. Parents must work closely with pediatricians to develop comprehensive management strategies that address both immediate symptoms and long-term health protection. Early intervention prevents these serious complications while supporting normal growth and development.
Read more: 7 Critical Baby Digestive Problems Every Parent Must RecognizeIntroducing Healthy First Foods
2. Pyloric Stenosis: The Hidden Baby Stomach Issue That Kills
Pyloric stenosis occurs when the muscle controlling food passage from the stomach to the small intestine thickens, creating a dangerous blockage that prevents proper nutrition and can lead to severe dehydration and death if untreated.
Critical Recognition Timeline: Symptoms typically appear between 2-8 weeks of age, beginning with occasional vomiting that progressively worsens to projectile vomiting after every feeding. The vomit doesn’t contain bile (remains white or clear) because food cannot pass beyond the stomach.
Emergency Warning Signs: Projectile vomiting that shoots several feet from the baby, visible stomach waves moving from left to right across the abdomen during feeding, constant hunger despite vomiting, rapid weight loss, and signs of severe dehydration including decreased urination and lethargy.
Treatment Urgency: Pyloric stenosis requires immediate surgical correction (pyloromyotomy). Delays in diagnosis and treatment can result in severe dehydration, electrolyte imbalances, and death. Parents must seek emergency medical care for any baby showing projectile vomiting patterns.
Pyloric Stenosis Diagnosis and Treatment Guidelines
3. Intussusception: The Emergency Infant Digestive Health Crisis
Intussusception occurs when one portion of intestine slides into an adjacent portion, creating a dangerous blockage that can cut off blood supply and cause tissue death. This condition represents a true pediatric emergency requiring immediate intervention.
Age-Specific Risks: While most common between 6 months to 3 years, intussusception can occur in younger babies, particularly those with underlying conditions. The condition often follows viral infections that cause lymph node swelling in the intestines.
Classic Symptom Triad: The combination of severe abdominal pain (causing babies to draw knees to chest and scream), vomiting that may become bile-stained, and “currant jelly” stools containing blood and mucus indicates possible intussusception requiring immediate emergency care.
The Danger of Misdiagnosis: Early symptoms can resemble stomach flu or colic, leading to dangerous delays in treatment. Between pain episodes, babies may seem relatively normal, which can mislead parents and even healthcare providers. Any baby with severe intermittent abdominal pain requires immediate medical evaluation.
4. Necrotizing Enterocolitis: The Devastating Premature Baby Threat
NEC primarily affects premature infants, causing portions of the intestinal wall to die, potentially leading to perforation, sepsis, and death. This condition represents one of the most serious digestive emergencies in neonatal intensive care.
High-Risk Populations: Babies born before 32 weeks gestation, those with very low birth weights, and infants with congenital heart conditions face the highest NEC risks. The condition rarely occurs in full-term babies but can develop in those with other risk factors.
Early Warning Signs: Feeding intolerance with increased residual stomach contents, abdominal distension and tenderness, blood in stool, lethargy, breathing difficulties, and temperature instability. These symptoms require immediate NICU evaluation and intervention.
Prevention Strategies: Breast milk feeding significantly reduces NEC risk compared to formula feeding. Probiotics may offer additional protection in high-risk infants, though their use should be discussed with neonatal specialists.
5. Infant Food Allergies: Hidden Dangers in Baby Nutrition
Food allergies in babies can range from mild digestive discomfort to life-threatening anaphylactic reactions. Early recognition and proper management are crucial for preventing serious complications and ensuring proper nutrition.
Milk Protein Allergy: The most common food allergy in infants, milk protein allergy can affect both formula-fed and breastfed babies (through maternal diet). Symptoms include bloody stools, severe colic, vomiting, poor weight gain, and eczema.
Milk Allergy Information from FARE
Multiple Food Protein Intolerance: Some babies develop intolerance to multiple proteins including milk, soy, and other common allergens. This condition can cause severe digestive symptoms and failure to thrive if not properly managed through dietary elimination.
Anaphylaxis Recognition: Severe food allergic reactions can cause difficulty breathing, swelling of face or throat, severe vomiting, and collapse. These symptoms require immediate emergency medical care and epinephrine administration.
The Rising Prevalence of Infant Food Sensitivities
Recent studies indicate that food allergies in babies have increased significantly over the past two decades, with current estimates suggesting approximately eight percent of children experience some form of food allergy during infancy. This dramatic rise highlights the importance of careful food introduction and vigilant symptom monitoring during the transition to solid foods.
Environmental factors, including changes in gut bacteria composition, delayed allergen exposure, and modern dietary patterns, may contribute to this increase. Parents with family histories of allergies, asthma, or eczema should exercise particular caution when introducing common allergenic foods including eggs, peanuts, tree nuts, fish, and shellfish.
Working with pediatric allergists to develop personalized introduction schedules helps minimize risks while ensuring adequate nutrition. Many specialists now recommend earlier introduction of certain allergens under medical supervision, contrary to previous recommendations for delayed exposure. This proactive approach may actually reduce allergy development in high-risk infants.
Read more: 7 Critical Baby Digestive Problems Every Parent Must RecognizeIntroducing Solid Foods Safely
6. Severe Baby Constipation and Hirschsprung Disease
While occasional constipation is common in babies, severe constipation or complete inability to pass stool can indicate serious underlying conditions requiring immediate medical attention.
Hirschsprung Disease: This congenital condition occurs when nerve cells are missing from parts of the intestine, preventing normal bowel movements. The condition affects 1 in 5,000 births and requires surgical correction.
Emergency Constipation Signs: No bowel movement within 48 hours of birth in newborns, severe abdominal distension, vomiting, and signs of intestinal obstruction require immediate medical evaluation. Chronic severe constipation can lead to toxic megacolon and intestinal perforation.
Differentiation from Normal Patterns: Breastfed babies may normally go several days without bowel movements, but they should not show signs of distress, abdominal distension, or feeding difficulties. When in doubt, seek medical evaluation.
7. Infectious Gastroenteritis: When Baby Stomach Issues Become Deadly
Viral and bacterial gastroenteritis can quickly cause life-threatening dehydration in babies due to their small fluid reserves and higher fluid requirements per body weight.
Rotavirus and Severe Dehydration: Before rotavirus vaccination, this virus was a leading cause of severe diarrhea and hospitalization in infants. Symptoms include profuse watery diarrhea, vomiting, and rapid dehydration.
Bacterial Infections: Salmonella, Campylobacter, and other bacterial pathogens can cause bloody diarrhea, high fever, and severe systemic illness in babies. These infections often require antibiotic treatment and hospitalization.
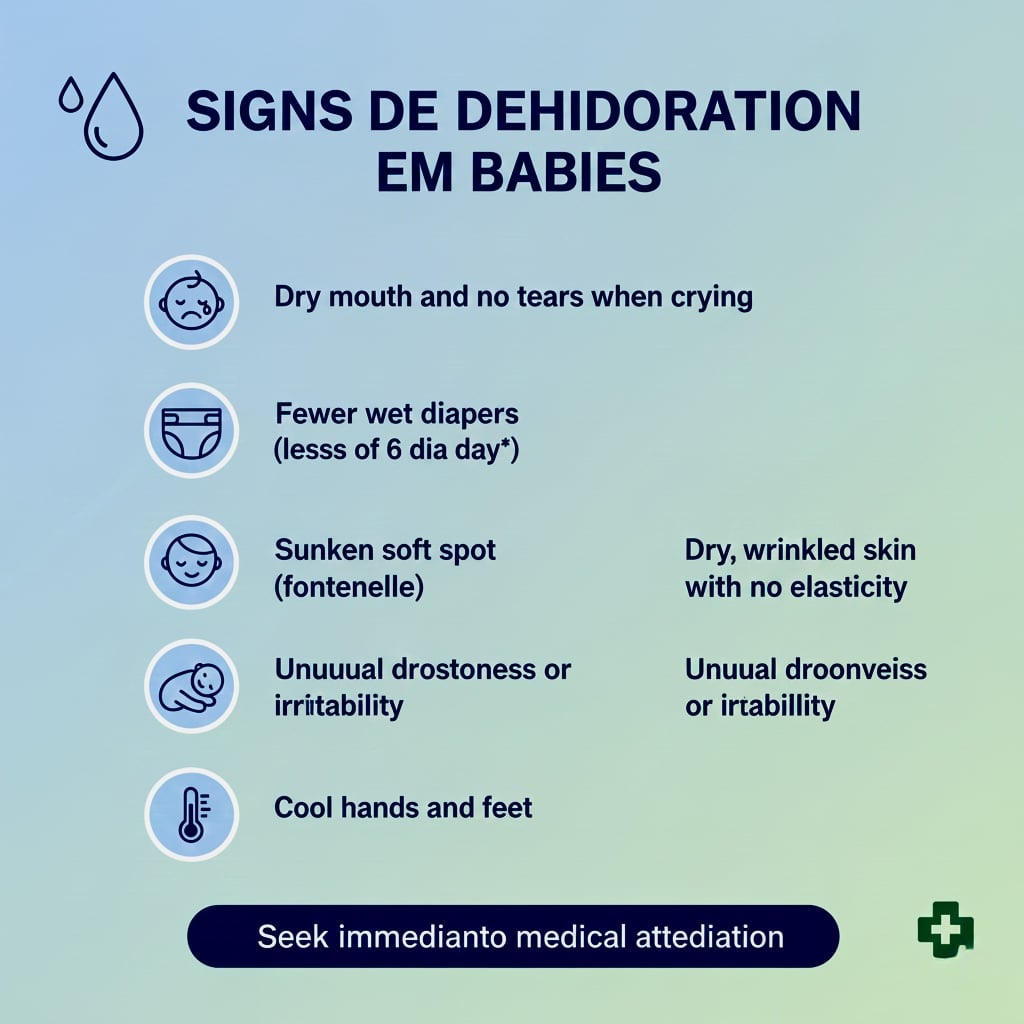
Dehydration Assessment: Signs of dangerous dehydration include decreased urination, dry mouth, sunken eyes or fontanelle, skin tenting, and decreased responsiveness. These symptoms require immediate medical intervention.
Signs of Dehydration in Infants
Recognizing Emergency Warning Signs of Baby Digestive Problems
Formula Preparation Errors: Incorrect formula mixing can cause serious digestive and systemic problems. Too concentrated formula can cause dehydration and kidney stress, while overly diluted formula can cause water intoxication and electrolyte imbalances.
Choking and Aspiration: Babies can aspirate milk or formula into their lungs, causing pneumonia or immediate breathing difficulties. Proper feeding positioning and pacing help prevent aspiration events.
Bottle Propping Dangers: Never prop bottles for unattended feeding, as this increases risks of choking, aspiration, and ear infections. Always hold babies during feeding for safety and bonding.
Creating a Digestive Health Protection Plan
Establishing Healthy Digestive Routines
Consistency in feeding schedules, sleep patterns, and daily routines significantly impacts digestive health throughout infancy. Babies thrive on predictability, and regular mealtimes help regulate digestive processes while making it easier to identify abnormal symptoms when they occur.
Maintaining detailed feeding logs during the first months allows parents to track intake volumes, frequency, and any concerning symptoms. These records prove invaluable during pediatric appointments, helping healthcare providers identify patterns that might indicate underlying digestive conditions. Document not only what and when your baby eats, but also diaper output, sleep quality, and behavioral changes that might signal digestive distress.
Breastfeeding Benefits for Infant Digestive Health:
Exclusive breastfeeding for the first six months provides optimal digestive health protection through beneficial bacteria, antibodies, and easily digestible nutrients. Breast milk also reduces risks of NEC, food allergies, and severe gastroenteritis.
Formula Safety and Baby Digestive Problems Prevention
When using formula, follow preparation instructions exactly, use proper sterilization techniques, and never save leftover formula between feedings. Store prepared formula safely and discard after recommended time periods.
Essential Baby Care and Feeding Guidance
Introduction of Solids: Follow your pediatrician’s guidance for introducing solid foods, typically around 6 months. Introduce single foods gradually to identify potential allergies or intolerances.
Recognizing Emergency Warning Signs of Baby Digestive Problems
Critical Symptoms Requiring Immediate Medical Care
Immediate Emergency Signs: Call 911 for severe breathing difficulties, signs of severe dehydration, blood in vomit or stool, severe abdominal distension, or any baby who becomes unresponsive or extremely lethargic.

Urgent Medical Attention: Seek prompt medical care for persistent vomiting, inability to keep fluids down for more than 8 hours, fever in babies under 3 months, or any significant change in feeding patterns or bowel movements.
Building Healthcare Relationships: Establish relationships with your pediatrician and know their after-hours policies. Many digestive emergencies develop gradually, making early professional consultation crucial for preventing serious complications.
Your vigilance in monitoring your baby’s digestive health can prevent minor issues from becoming life-threatening emergencies. Trust your parental instincts, maintain regular pediatric care, and never hesitate to seek medical attention when concerned about your baby’s digestive symptoms. The knowledge and confidence you develop in protecting your baby’s digestive health will serve as a foundation for their lifelong wellness and development.
Monitoring Your Baby’s Sleep and Health Patterns
Conclusion:
Remember that you know your baby better than anyone else. Trust your parental instincts when something seems wrong, even if you cannot precisely identify the problem. Pediatricians value parental observations and concerns, recognizing that caregivers often detect subtle changes that indicate serious conditions requiring immediate evaluation and treatment.
Looking for comprehensive guidance on caring for your baby? Our book ‘How to Care for Children: From Birth to Age 2’ combines professional nanny experience with evidence based child development research. Written by Kelly and Peter, this guide provides clear, reliable advice rooted in real world childcare. Available in English, Spanish, and Portuguese on Amazon.
Click the link below your preferred language to get your copy!

1. What are the most common baby digestive problems in newborns?
The most common baby digestive problems include gastroesophageal reflux (GERD in babies), colic, baby constipation, and infant food allergies. Most newborns experience some degree of spitting up due to immature digestive systems, but severe symptoms require medical evaluation to protect infant digestive health.
2. When should I worry about baby stomach issues?
Seek immediate medical care for baby digestive problems if you notice projectile vomiting, blood in stool or vomit, signs of severe dehydration, extreme lethargy, high fever in babies under 3 months, or inability to keep fluids down for more than 8 hours. These symptoms may indicate serious infant digestive health emergencies.
3. How can I tell if my baby has GERD or normal reflux?
While normal infant reflux involves occasional spitting up without discomfort, GERD in babies causes severe symptoms including projectile vomiting, poor weight gain, chronic coughing, back arching during feeds, and obvious pain. If baby digestive problems interfere with feeding or growth, consult your pediatrician immediately.
4. What causes baby constipation and when is it dangerous?
Baby constipation can result from formula changes, dehydration, or introduction of solid foods. However, severe baby stomach issues like Hirschsprung disease cause dangerous constipation requiring surgery. Seek medical attention if your newborn has no bowel movement within 48 hours of birth or shows severe abdominal distension.
5. Can breastfeeding prevent baby digestive problems?
Breastfeeding significantly reduces risks of many baby digestive problems including necrotizing enterocolitis, severe gastroenteritis, and infant food allergies. Breast milk provides beneficial bacteria, antibodies, and easily digestible nutrients that protect infant digestive health during critical development periods.
6. What are emergency warning signs of baby digestive problems?
Call 911 for severe breathing difficulties, extreme dehydration signs, bloody vomit or stool, severe abdominal swelling, or unresponsiveness. These baby stomach issues require immediate emergency intervention to prevent life-threatening complications affecting infant digestive health.
7. How do I know if my baby has a food allergy?
Infant food allergies may cause bloody stools, severe vomiting, poor weight gain, eczema, or breathing difficulties. The most common trigger is milk protein allergy affecting both formula-fed and breastfed babies. Severe allergic reactions causing swelling, breathing problems, or collapse require immediate emergency care.
8. What is the difference between pyloric stenosis and normal vomiting?
Pyloric stenosis causes forceful projectile vomiting that shoots several feet from the baby after every feeding, typically appearing between 2 to 8 weeks of age. Unlike normal baby digestive problems, this condition shows visible stomach waves and requires emergency surgical correction to prevent life-threatening dehydration.
Want a complete baby care guide?
Get our FREE checklist sent directly to your inbox - covering everything from birth to age 2, including daily routines, safety guidelines, and developmental milestones.
- ✅ Birth to 3 months essentials
- ✅ 4-12 months routines & alerts
- ✅ 1-2 years development & safety
Enter your email to receive instant access to the PDF