Learn to identify 7 dangerous skin conditions in babies that require immediate medical care. Recognize emergency signs and protect your infant’s health.
Your baby’s delicate skin serves as their first line of defense against the outside world, yet it can also become the battleground for serious medical conditions that masquerade as harmless rashes or minor irritations. As a parent, distinguishing between normal skin changes and potentially life-threatening conditions can feel overwhelming, especially when what appears to be a simple diaper rash or birthmark could actually signal a medical emergency requiring immediate intervention.
The terrifying reality is that babies’ immature immune systems and sensitive skin make them vulnerable to rapidly progressing conditions that can escalate from seemingly innocent spots to systemic infections, organ failure, or death within hours. Many dangerous skin conditions in infants present with subtle early symptoms that even experienced parents and healthcare providers can initially overlook, making early recognition absolutely critical for your baby’s survival.
This essential guide will transform you from an anxious observer into a knowledgeable guardian capable of recognizing when your baby’s skin symptoms represent true medical emergencies that demand immediate professional attention.
Understanding Why Babies Develop Dangerous Skin Conditions
The Vulnerability of Infant Skin to Emergency Conditions
Infant skin differs dramatically from adult skin in ways that create unique vulnerabilities to serious conditions. Babies are born with skin that is 40-60% thinner than adult skin, with an underdeveloped protective barrier that allows pathogens and irritants to penetrate more easily. Additionally, their immune systems are still developing, making them less capable of fighting off infections that could remain localized in older children and adults.
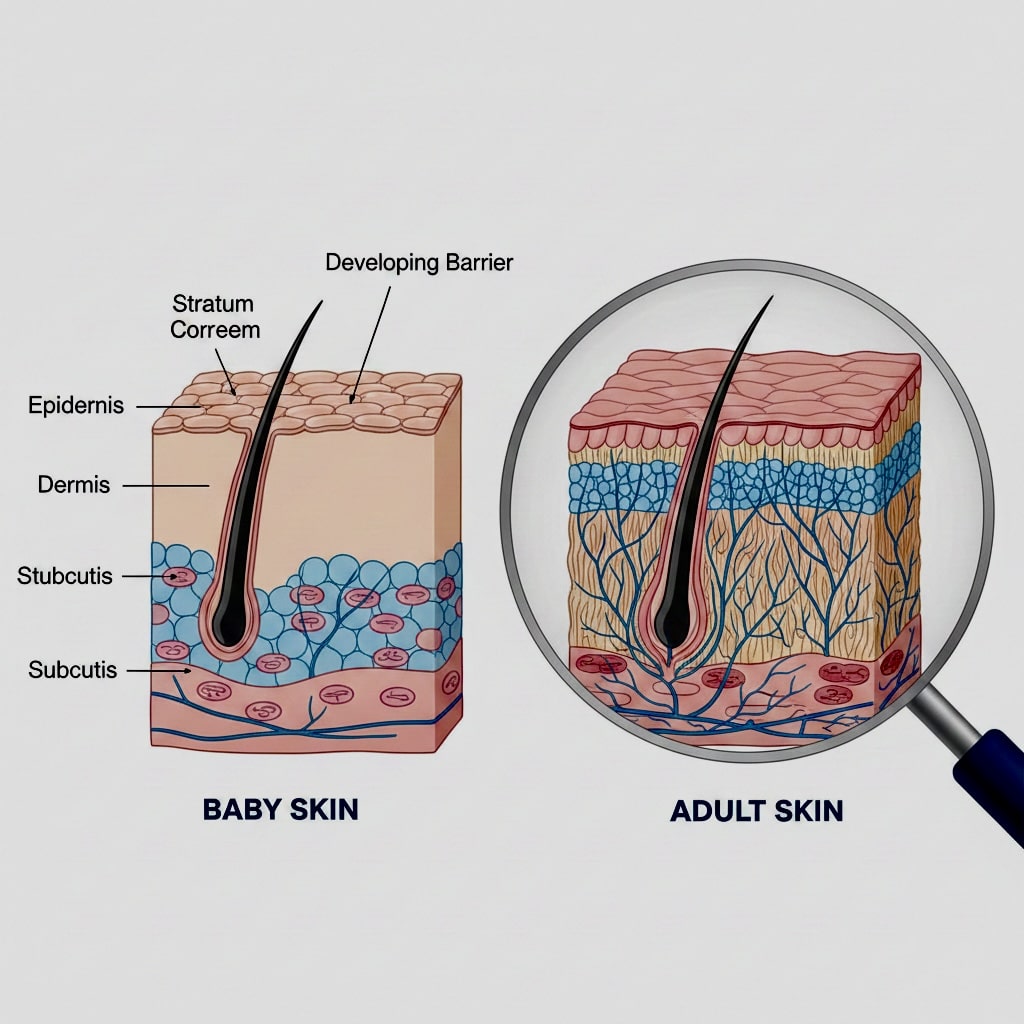
The American Academy of Dermatology emphasizes that newborn and infant skin undergoes rapid changes during the first year of life, making it crucial for parents to understand which changes are normal development and which represent dangerous conditions requiring immediate medical attention.
Furthermore, babies’ small body surface area means that localized skin infections can quickly become systemic, affecting vital organs and causing life-threatening complications much faster than in larger children or adults.
1 – Necrotizing Fasciitis in Babies: The Flesh-Eating Emergency
Necrotizing fasciitis represents one of the most dangerous skin and soft tissue infections that can affect babies, progressing from initial symptoms to life-threatening complications within 12-24 hours. This aggressive bacterial infection destroys skin, fat, and muscle tissue, requiring immediate surgical intervention and intensive antibiotic therapy.
Necrotizing fasciitis treatment guidelines
Early Recognition Challenges in Infant Skin Infections:
Initial symptoms often resemble cellulitis or simple skin infections, beginning with redness, warmth, and swelling that may seem like minor irritation. However, necrotizing fasciitis progresses rapidly, with skin becoming increasingly painful, developing purple or black discoloration, and potentially showing skin breakdown or blistering.
Critical Warning Signs of Baby Skin Emergencies
Severe pain that seems disproportionate to the appearance of the infection, rapid spreading of redness or discoloration, skin that feels hard or woody to touch, fever and signs of systemic illness, and areas of skin that become numb or develop blisters or bullae.
Emergency Response Requirements
Any suspicion of necrotizing fasciitis requires immediate emergency medical care. Delays in treatment can result in amputation, organ failure, or death. The condition requires aggressive surgical debridement and high-dose intravenous antibiotics.
Just as you monitor for dangerous skin conditions in babies, you should also be aware of serious baby health conditions requiring immediate attention that affect the digestive system.
High-Risk Situations: Babies with compromised immune systems, recent surgical procedures, or traumatic injuries face higher risks. However, necrotizing fasciitis can occur in otherwise healthy infants following minor cuts, insect bites, or even without obvious injury points.
2 – Staphylococcal Scalded Skin Syndrome: A Life-Threatening Baby Rash
SSSS is a serious condition caused by toxins produced by certain strains of Staphylococcus aureus bacteria, causing widespread skin peeling and blistering that can resemble severe burns. This condition primarily affects children under 2 years old and can be life-threatening if not promptly treated.
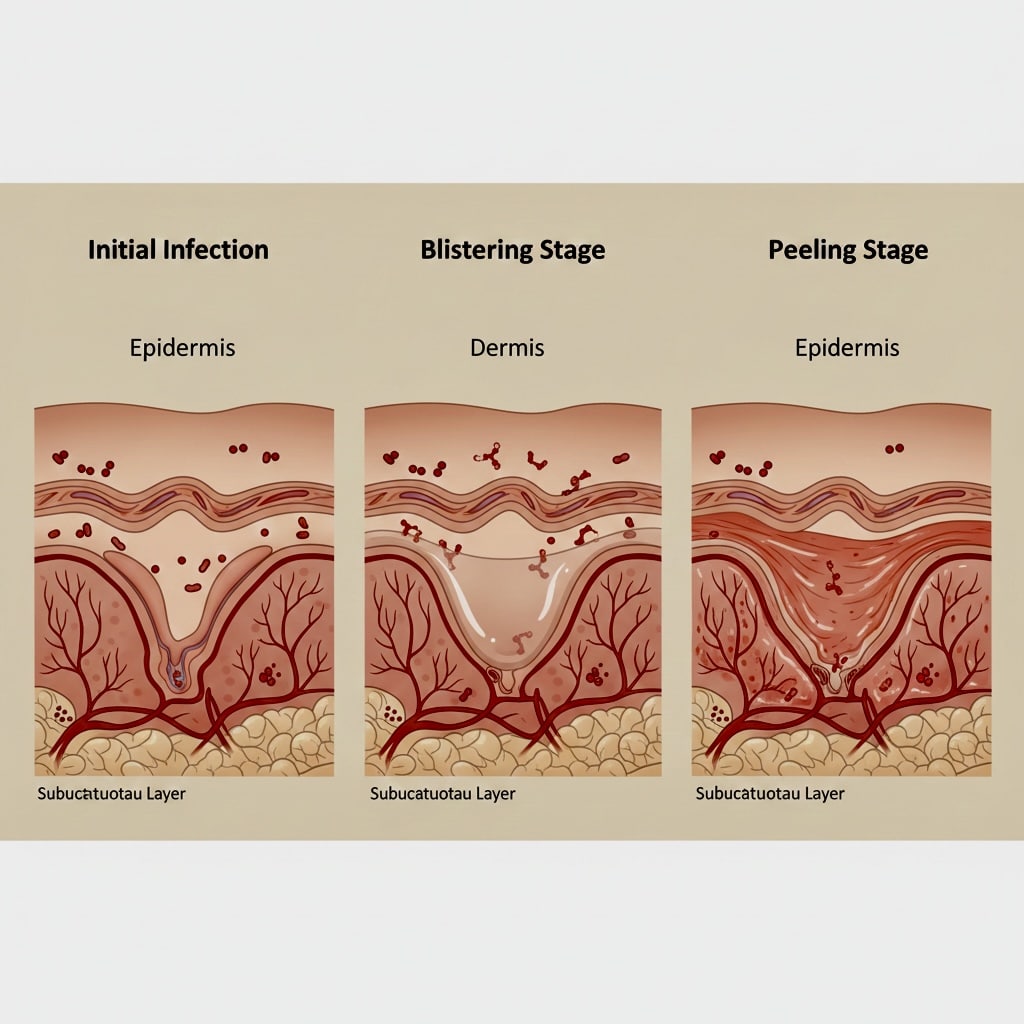
Progression Pattern of Emergency Baby Skin Problems
SSSS typically begins with fever, irritability, and skin tenderness, followed by the development of a widespread red rash that may initially resemble sunburn. Within 24-48 hours, the skin begins to wrinkle and peel in large sheets, particularly around the mouth, nose, and diaper area.
Nikolsky’s Sign: Key Diagnostic Feature
A key diagnostic feature is positive Nikolsky’s sign, where gentle pressure or rubbing of the skin causes it to separate and peel away from underlying layers. This finding indicates the serious nature of the condition and need for immediate medical care.
Complications and Treatment: SSSS can lead to severe dehydration, secondary bacterial infections, and sepsis if untreated. Treatment requires hospitalization with intravenous antibiotics and careful fluid management. The condition can be fatal in young infants if not recognized and treated promptly.
Differentiation from Other Conditions: SSSS must be distinguished from toxic epidermal necrolysis, chemical burns, and other blistering conditions. Prompt medical evaluation is essential for accurate diagnosis and appropriate treatment.
3 – Meningococcal Disease: When a Baby Rash Signals Death
Meningococcal disease can present with a characteristic skin rash that represents a medical emergency requiring immediate intervention. The rash associated with meningococcemia indicates bacterial infection of the bloodstream and can progress to shock and death within hours.
Rash Characteristics in Dangerous Skin Conditions in Babies
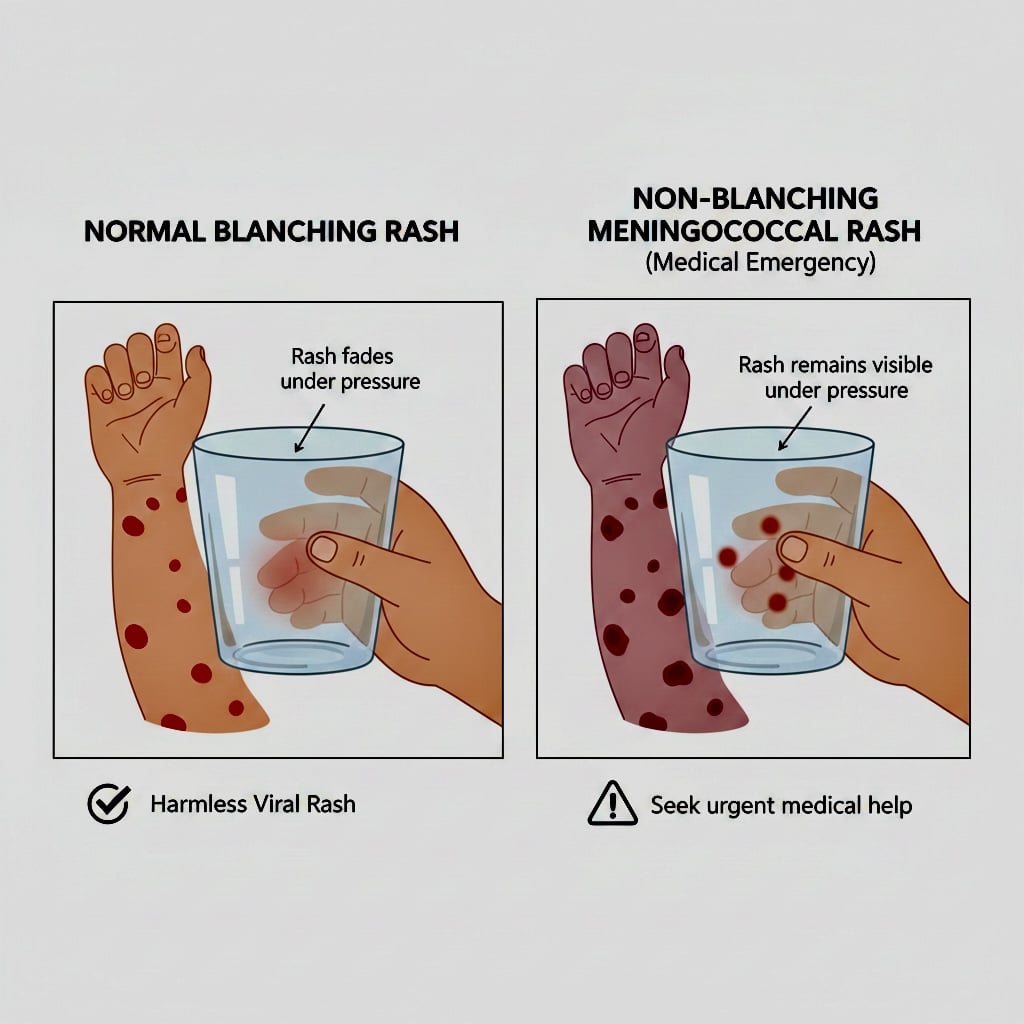
The meningococcal rash typically begins as small, red or purple spots that don’t fade when pressed with a glass (non-blanching petechiae). These spots may rapidly increase in size and number, sometimes developing into larger purple or black areas of skin.
The Glass Test for Baby Skin Emergencies
Parents should perform the “glass test” by pressing a clear glass against suspicious spots. If the spots remain visible through the glass and don’t fade with pressure, this suggests meningococcal disease and requires immediate emergency medical care.
Associated Symptoms: The rash may be accompanied by fever, severe headache, neck stiffness, nausea, vomiting, sensitivity to light, and rapid deterioration in the child’s overall condition. However, not all symptoms may be present, especially in very young infants.
Time-Critical Treatment: Meningococcal disease can progress from initial symptoms to death within 4-6 hours. Immediate antibiotic treatment and supportive care are essential for survival. Any suspicion of meningococcal rash requires immediate emergency medical attention.
4 – Kawasaki Disease: Multi-System Infant Skin Infections
Kawasaki disease is a serious inflammatory condition affecting blood vessels throughout the body, with characteristic skin changes that can help with early recognition. While the skin manifestations may seem minor, untreated Kawasaki disease can cause permanent heart damage.
Skin and Mucous Membrane Changes
Key features include conjunctival redness without discharge, red and cracked lips, “strawberry tongue” with prominent red bumps, rash on the trunk and extremities, and changes to hands and feet including redness, swelling, and later peeling of fingertips and toes.
Diagnostic Criteria: Kawasaki disease diagnosis requires fever lasting 5 or more days plus at least four of the characteristic features. The combination of symptoms, rather than any single finding, suggests the diagnosis.
Cardiac Complications from Emergency Baby Skin Problems
The most serious complication is coronary artery damage, which can occur in up to 25% of untreated children. Early treatment with intravenous immunoglobulin and aspirin significantly reduces this risk.
Treatment Window: Treatment must be initiated within 10 days of fever onset to prevent cardiac complications. Parents should seek medical evaluation for prolonged fever with any of the characteristic skin or mucous membrane changes.
5 – Stevens-Johnson Syndrome: Severe Infant Skin Infections
These severe skin reactions can be triggered by medications, infections, or other factors, causing widespread skin and mucous membrane damage that can be life-threatening in infants.
Clinical Presentation of Life-Threatening Baby Rash
Both conditions begin with fever and flu-like symptoms, followed by the development of painful red or purple skin lesions that progress to blistering and skin sloughing. Mucous membranes of the mouth, eyes, and genitals are typically involved.
Severity Differences: Stevens-Johnson syndrome affects less than 10% of body surface area, while toxic epidermal necrolysis affects more than 30%. Both conditions require immediate medical attention and often intensive care management.
Common Triggers: In infants, these conditions may be triggered by viral infections, though medication reactions become more common as children age and are exposed to more drugs. Some cases occur without identifiable triggers.
Management Requirements for Baby Skin Emergencies
Treatment involves discontinuing potential triggering agents, supportive care similar to burn management, and sometimes immunosuppressive therapy. The conditions carry significant mortality risk, especially in young infants.
6 – Infantile Hemangiomas: When Birthmarks Become Dangerous Skin Conditions in Babies
While most hemangiomas are harmless vascular birthmarks, certain types and locations can cause serious complications requiring immediate medical intervention.
Airway-Threatening Hemangiomas
Hemangiomas located around the mouth, nose, or neck can grow rapidly and obstruct breathing passages. These lesions require immediate evaluation and often urgent treatment to prevent respiratory compromise.
PHACE Syndrome and Associated Risks
Large facial hemangiomas may be associated with PHACE syndrome, involving abnormalities of the posterior fossa brain structures, arterial anomalies, cardiac defects, eye abnormalities, and sternal defects. This condition requires comprehensive medical evaluation and management.
Ulceration and Bleeding: Large or rapidly growing hemangiomas can develop ulcerations that become infected or bleed significantly. These complications require prompt medical attention and sometimes surgical intervention.
Treatment Considerations: Problematic hemangiomas may require treatment with propranolol, laser therapy, or surgical intervention. Early consultation with pediatric specialists is important for optimal outcomes.
7 – Congenital Melanocytic Nevi: The Cancer Risk in Babies
Large congenital melanocytic nevi (birthmarks composed of pigment cells) carry risks of malignant transformation that require careful monitoring and sometimes prophylactic removal.
Modern technology helps parents in monitoring your baby’s overall health and patterns, including changes in behavior that might indicate illness.
Size Classifications: Giant congenital nevi (projected adult size >20 cm) carry the highest cancer risk, with melanoma developing in 5-10% of cases, often during childhood. Smaller lesions carry lower but still significant risks.
Neurocutaneous Melanosis: Large nevi, especially those on the back or head, may be associated with melanin deposits in the brain and spinal cord, potentially causing seizures, developmental delays, or other neurological problems.
Monitoring Protocols: All congenital nevi require regular dermatologic surveillance for changes in color, texture, or growth patterns that might suggest malignant transformation. Large lesions often require MRI screening for neurocutaneous involvement.
Treatment Decisions: Management decisions depend on size, location, and associated risks. Some large nevi may require staged surgical removal, while others can be monitored with regular examinations and photography.
Recognizing Emergency Baby Skin Problems: When to Seek Immediate Care
Immediate Emergency Signs of Dangerous Skin Conditions in Babies
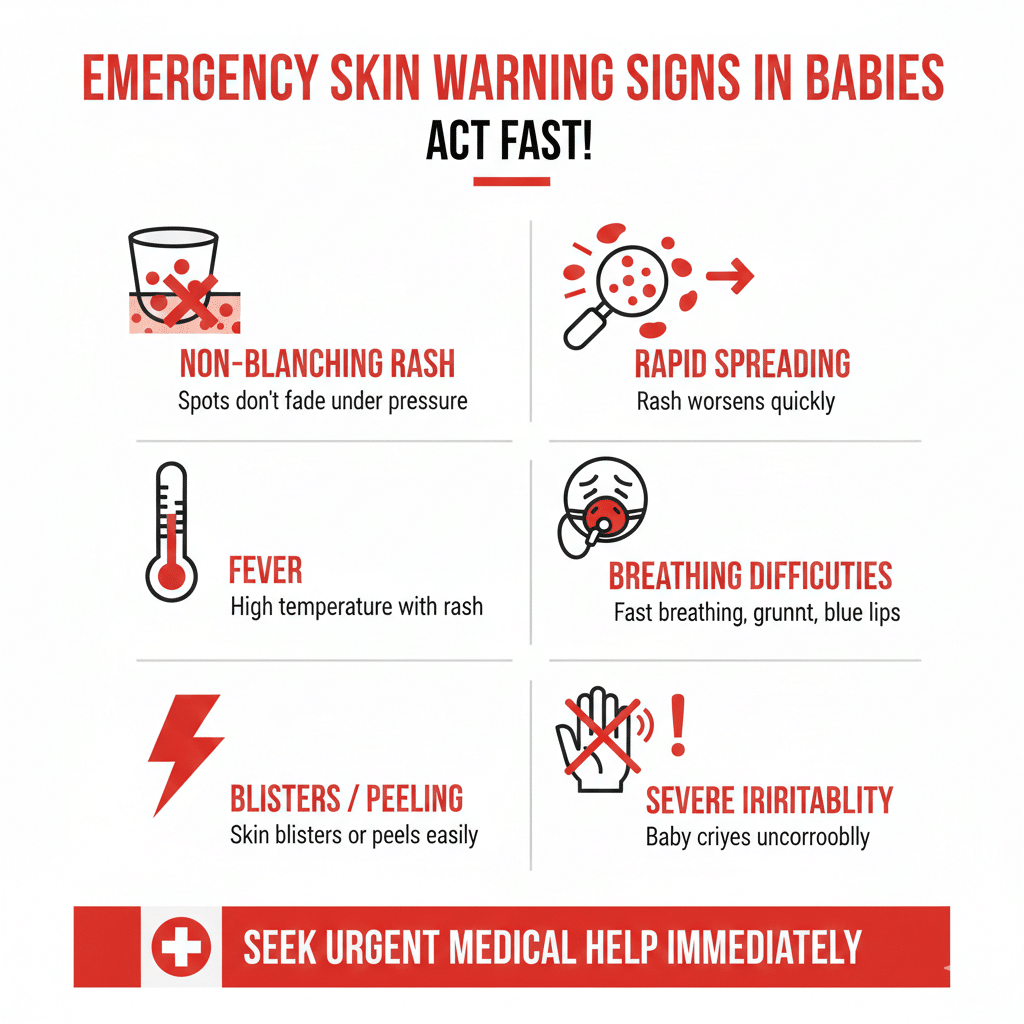
Call 911 for any rash that doesn’t fade with pressure (glass test), signs of severe systemic illness with skin changes, rapid spreading of skin infection, skin that appears necrotic or black, or breathing difficulties associated with facial or neck swelling.
When Infant Skin Infections Require Urgent Medical Attention
Seek prompt medical care for fever with characteristic rashes, painful skin lesions with blistering, any rash associated with severe illness, rapid changes in existing birthmarks, or any skin condition causing significant distress or interfering with feeding or breathing.
Documentation Strategy for Baby Skin Emergencies
Photograph concerning skin changes to track progression and provide visual information to healthcare providers. This documentation can be crucial for accurate diagnosis and treatment planning.
Building Awareness and Prevention of Dangerous Skin Conditions in Babies
Regular Skin Examination for Early Detection
Develop habits of regularly examining your baby’s skin during diaper changes and bath time. Familiarity with your baby’s normal skin helps you recognize concerning changes early and prevent life-threatening baby rash complications.
Building your baby’s immune system through healthy nutrition for your baby’s immune system helps protect against infections that can manifest as skin conditions.
Sun Protection Against Emergency Baby Skin Problems
Even brief sun exposure can damage infant skin. Use appropriate sun protection, avoid direct sunlight for babies under 6 months, and monitor for any unusual reactions to sun exposure.
Gentle Skin Care: Use mild, fragrance-free products specifically designed for infant skin. Avoid harsh chemicals, excessive bathing, and products that could trigger allergic reactions.
Choosing safe baby skin care products designed specifically for infant skin helps prevent irritation and allergic reactions.
Having the right essential baby care items makes it easier to maintain proper hygiene and skin care routines that prevent infections.
Professional Relationships for Managing Infant Skin Infections
Establish relationships with pediatric dermatologists or knowledgeable pediatricians who can evaluate concerning skin changes promptly. Early professional consultation often prevents minor issues from becoming serious complications.
Your vigilance in monitoring your baby’s skin health can literally save their life by ensuring prompt recognition and treatment of dangerous conditions. Trust your parental instincts, document concerning changes, and never hesitate to seek immediate medical attention when your baby’s skin shows signs of serious illness. The knowledge you gain about recognizing dangerous skin conditions will serve as lifelong protection for your child’s health and well-being.
While caring for your newborn involves vigilance about health concerns, it also includes building loving routines and connections.
Looking for comprehensive guidance on caring for your baby? Our book ‘How to Care for Children: From Birth to Age 2’ combines professional nanny experience with evidence based child development research. Written by Kelly and Peter, this guide provides clear, reliable advice rooted in real world childcare. Available in English, Spanish, and Portuguese on Amazon.
Click the link below your preferred language to get your copy!

1. What are the most dangerous skin conditions in babies?
The most dangerous skin conditions in babies include necrotizing fasciitis (flesh-eating bacteria), meningococcal disease with characteristic rash, Staphylococcal Scalded Skin Syndrome (SSSS), Stevens-Johnson Syndrome, and Kawasaki disease. These conditions can progress rapidly and require immediate medical intervention to prevent serious complications or death.
2. How can I tell if my baby’s rash is an emergency?
Perform the glass test by pressing a clear glass against the rash. If spots don’t fade with pressure, seek emergency care immediately. Other emergency signs include rapid spreading of redness, skin that appears black or necrotic, severe pain, high fever, breathing difficulties, or any rash accompanied by severe illness symptoms.
3. What is the glass test for baby rashes?
The glass test involves pressing a clear drinking glass firmly against your baby’s skin rash. If the spots or rash fade and disappear when pressed, it’s usually less concerning. However, if the spots remain visible through the glass (non-blanching), this could indicate meningococcal disease or other serious conditions requiring immediate emergency medical care.
4. Can infant skin infections become life-threatening quickly?
Yes, infant skin infections can progress to life-threatening conditions within hours due to babies’ immature immune systems and thin skin barriers. Conditions like necrotizing fasciitis can advance from initial symptoms to severe complications in 12 to 24 hours, while meningococcal disease can progress to shock and death within 4 to 6 hours.
5. When should I take my baby to the emergency room for a skin condition?
Take your baby to the emergency room immediately if you notice a non-blanching rash (doesn’t fade with glass test), rapidly spreading skin infection, black or necrotic appearing skin, severe pain with skin changes, breathing difficulties with facial swelling, or any rash accompanied by high fever and severe illness symptoms.
6. Are all baby rashes harmless?
No, while many baby rashes are harmless and resolve on their own, some rashes indicate serious medical emergencies. Life-threatening baby rash conditions include those associated with meningococcal disease, SSSS, necrotizing fasciitis, and Stevens-Johnson Syndrome. Always consult your pediatrician if you’re uncertain about any rash.
7. What causes dangerous skin conditions in babies?
Dangerous skin conditions in babies can be caused by bacterial infections (necrotizing fasciitis, SSSS, meningococcal disease), viral infections, immune system reactions, medication reactions (Stevens-Johnson Syndrome), or inflammatory conditions (Kawasaki disease). Babies’ immature immune systems and thinner skin make them more vulnerable to these serious conditions.
8. How quickly do emergency baby skin problems develop?
Emergency baby skin problems can develop extremely rapidly. Necrotizing fasciitis progresses in 12 to 24 hours, meningococcal disease can advance to critical stages in 4 to 6 hours, and SSSS develops widespread peeling within 24 to 48 hours. This rapid progression makes early recognition and immediate medical attention crucial for your baby’s survival.