Critical Statistics About Emergency Eye and Ear Infections in Babies
- 1 in 4 babies experience ear infections before age 2
- Emergency eye infections affect 0.3% of newborns annually
- 85% of cases are preventable with early recognition
- Delayed treatment increases complications risk by 300%
Emergency Eye and Ear Infections in Babies are among the most dangerous yet overlooked conditions parents may face. These 5 emergency eye and ear infections in babies can progress within hours, leading to irreversible hearing loss in infants or permanent vision loss in babies if not recognized and treated quickly.
⚠️ EMERGENCY WARNING
If your baby shows signs of any of these 5 emergency eye and ear infections, seek immediate medical attention. These conditions can cause permanent damage within hours.
Creating meaningful family traditions with your new baby.
Your baby’s developing sensory systems represent irreplaceable windows to the world, yet they remain heartbreakingly vulnerable to infections that can steal sight or hearing forever within hours of onset. As a parent, distinguishing between common childhood eye discharge or ear discomfort and sight-threatening or hearing-destroying emergencies can feel overwhelming, especially when your infant cannot verbalize their pain or describe what they’re experiencing.
The devastating reality is that serious cases among the 5 emergency eye and ear infections in babies can progress from mild symptoms to permanent sensory damage with terrifying speed, often while parents dismiss early warning signs as normal childhood ailments. Unlike adults who can describe their symptoms and seek help independently, babies depend entirely on their caregivers to recognize when routine infections become medical emergencies requiring immediate intervention to save their vision or hearing.
Recognizing the signs of emergency eye and ear infections in babies can save your child’s sight and hearing. This critical guide will transform you from an anxious observer into a knowledgeable guardian capable of recognizing when your baby’s eye or ear symptoms signal true medical emergencies that demand Fimmediate professional attention to prevent lifelong disabilities.
Quick Reference: The 5 Emergency Eye and Ear Infections in Babies
| Infection | Onset Time | Severity | Action Needed |
|---|---|---|---|
| Orbital Cellulitis | 12-24 hours | Critical | Emergency room immediately |
| Endophthalmitis | 6-12 hours | Severe | Urgent specialist care |
| Mastoiditis | 48-72 hours | High | Hospital admission |
| Complicated Otitis Media | 24-48 hours | Moderate-High | Urgent pediatric care |
| Neonatal Conjunctivitis | Birth-7 days | Variable | Same-day evaluation |

Understanding the 5 Emergency Eye and Ear Infections in Babies
Parents must recognize that the 5 emergency eye and ear infections in babies require different treatment approaches.
Baby’s eyes and ears undergo rapid development during the first years of life, making them particularly susceptible to infections that could permanently damage these delicate structures. The immune systems protecting these sensory organs are still maturing, creating windows of vulnerability where bacterial, viral, or fungal infections can cause irreversible harm.
Infants are especially vulnerable to Emergency Eye and Ear Infections in Babies because their sensory systems are still developing.
The American Academy of Pediatrics emphasizes that infant eye and ear anatomy differs significantly from adult structures.
Unlike older children, babies have immature tear ducts and eustachian tubes, that don’t drain effectively making them more prone to infections that can escalate quickly into medical emergencies and thinner protective barriers that allow pathogens to penetrate more easily. These developmental factors mean that infections can spread rapidly and cause more severe complications than similar infections in older children or adults.
Hearing loss in infants: Additionally, babies’ small anatomical structures mean that even minor swelling or inflammation can cause significant functional impairment, blocking drainage pathways or compressing vital structures in ways that can quickly lead to serious complications.
Age-Specific Risk Factors for Eye and Ear Infections in Babies
Understanding how susceptibility to eye and ear infections in babies changes with age helps parents recognize when their infant faces heightened risks requiring extra vigilance. The developmental stage of your baby’s immune system and anatomical structures significantly influences both infection risk and severity.
Newborns (0-28 Days): Critical Vulnerability Period
Newborns face unique risks for eye and ear infections in babies due to immature immune systems and potential exposure to pathogens during birth. This age group requires immediate medical evaluation for any concerning eye or ear symptoms.
Birth-Acquired Eye and Ear Infections in Babies: Neonatal conjunctivitis represents one of the most serious eye infections in newborns, potentially acquired from maternal genital infections during vaginal delivery. Chlamydia and gonorrhea infections can cause severe eye damage within hours if not treated immediately after birth. Standard prophylactic eye drops given at birth help prevent these dangerous eye and ear infections in babies.
Immune System Limitations: Newborns lack mature immune responses, making even mild-appearing infections potentially dangerous. Eye and ear infections in babies during this period can rapidly progress to systemic infections affecting multiple organ systems. Maternal antibodies provide some protection, but gaps in immunity leave newborns vulnerable to specific pathogens.
Anatomical Vulnerabilities: Tear ducts in newborns often don’t fully open until several weeks after birth, creating blockages that can lead to eye and ear infections in babies. The eustachian tubes connecting middle ears to the throat are shorter and more horizontal than in older children, facilitating bacterial migration and increasing risk for ear infections.
Red Flag Symptoms in Newborns: Any eye discharge beyond minimal tearing, swelling of eyelids, redness of the eye white, or drainage from ears requires same-day pediatric evaluation. Don’t dismiss symptoms as normal in newborns, as eye and ear infections in babies this young can cause permanent damage within hours.
Young Infants (1-6 Months): Developing Immunity
As babies transition beyond the newborn period, their immune systems begin maturing, but significant vulnerabilities to eye and ear infections in babies remain during this critical developmental stage.
Respiratory Infection Connections: Upper respiratory infections become more common as babies encounter environmental pathogens. These viral infections create conditions favoring secondary bacterial eye and ear infections in babies. Congestion blocks tear ducts and eustachian tubes, creating ideal environments for bacterial overgrowth.
Feeding Position Impact: Bottle-feeding in supine positions increases risk for ear infections as milk can flow back through eustachian tubes. While this doesn’t directly cause eye and ear infections in babies, it creates conditions promoting bacterial growth in middle ears. Proper feeding positions reduce this risk.
Daycare Exposure: Infants in group care settings face dramatically increased exposure to pathogens causing eye and ear infections in babies. Close contact with other children facilitates transmission of viruses and bacteria that can lead to serious infections requiring emergency treatment.
Developmental Milestones: As babies begin exploring their environment through touch and bringing objects to mouths, they encounter more pathogens that can cause eye and ear infections in babies. Hand-to-eye contact transfers bacteria that can lead to conjunctivitis and other infections.
Older Infants (6-12 Months): Peak Infection Period
The second half of the first year represents peak vulnerability for certain eye and ear infections in babies as maternal antibodies decline before babies’ own immune systems fully mature.
Teething Complications: While teething doesn’t directly cause eye and ear infections in babies, the process creates inflammation and increased drooling that can affect eustachian tube function. Babies also tend to touch their faces more during teething, potentially introducing bacteria to eyes and ears.
Crawling and Exploration: Mobile babies encounter floor-level dirt, pet dander, and other allergens and irritants that can contribute to eye and ear infections in babies. Increased environmental exposure combined with frequent hand-to-face contact creates multiple infection pathways.
Sleep Position Changes: As babies learn to roll and change positions during sleep, their drainage patterns change. Some positions promote better ear drainage while others may contribute to fluid accumulation increasing risk for ear infections.
Social Interaction Expansion: Increased interaction with siblings, relatives, and other children exposes babies to respiratory viruses that commonly precede bacterial eye and ear infections in babies. Each viral infection creates opportunities for secondary bacterial complications.
Toddlers (12-24 Months): Persistent Vulnerabilities
Even as children approach their second birthday, anatomical and behavioral factors continue creating risks for eye and ear infections in babies that require parental awareness and prompt treatment.
Communication Challenges: Toddlers cannot clearly communicate pain or discomfort, making early detection of eye and ear infections in babies difficult. Parents must rely on behavioral changes like increased crying, sleep disruption, or decreased appetite to recognize potential infections.
Continuing Anatomical Immaturity: Eustachian tubes don’t reach adult configuration until around age 7, meaning toddlers still face elevated risks for ear infections compared to older children. Eye structures continue developing, maintaining some vulnerability to serious eye and ear infections in babies.
Antibiotic Resistance Considerations: Toddlers with multiple prior infections may harbor antibiotic-resistant bacteria, complicating treatment of new eye and ear infections in babies. This resistance pattern makes prevention through vaccination and hygiene particularly important.
Seasonal Variations: Winter months bring increased rates of eye and ear infections in babies due to indoor crowding, respiratory virus circulation, and reduced ventilation. Parents should maintain extra vigilance during cold and flu season.
More information: Ear Infections in Children: Information for Parents – Health Children.org
Symptoms Checklist: 5 Emergency Eye and Ear Infections in Babies
Immediate Emergency (Call 911):
- [ ] Sudden vision loss
- [ ] Eye bulging forward
- [ ] Severe swelling behind ear
- [ ] High fever with altered consciousness
- [ ] Signs of meningitis
Urgent Care (Within 2 Hours):
- [ ] Inability to move eye normally
- [ ] Severe eye pain with fever
- [ ] Persistent ear drainage
- [ ] Facial paralysis
- [ ] Rapid symptom progression
#1 Orbital Cellulitis: Vision-Threatening Emergency Eye Infection
Permanent Vision and Hearing Loss in Babies: Orbital cellulitis is one of the most dangerous forms of Emergency Eye and Ear Infections in Babies, capable of causing blindness within hours if left untreated. Parents often mistake early signs for simple conjunctivitis, which delays proper treatment.
Recognizing the Progression: Orbital cellulitis typically begins with symptoms that may resemble simple conjunctivitis or a stye, including redness, swelling, and discharge. However, the condition rapidly progresses to involve deeper tissues, causing severe swelling that can completely close the eye, restriction of eye movement, and protrusion of the eyeball.
Critical Warning Signs: Key indicators include swelling that extends beyond the eyelid to involve the entire eye area, inability to move the eye normally in all directions, double vision, decreased vision, fever, and severe pain with eye movement. The affected eye may appear to bulge forward, and the child may seem systemically ill with high fever and lethargy.
Complications and Urgency: Untreated orbital cellulitis can lead to permanent vision loss, brain abscess, meningitis, and death. The infection can spread along nerve pathways to reach the brain, creating life-threatening complications within hours. Immediate hospitalization with intravenous antibiotics and sometimes surgical drainage is essential.
Risk Factors: Children with recent sinus infections, dental infections, or upper respiratory infections face higher risks. The condition can also develop following minor injuries around the eye or from spread of more superficial skin infections.
Proper newborn hygiene practices
#2 Endophthalmitis: Critical Eye Infection Emergency in Babies
Permanente vision and Hearing Loss in Baby advice: Endophthalmitis involves infection inside the eyeball itself, affecting the vitreous humor and potentially destroying all vision in the affected eye if not treated within hours of onset. This condition represents a true ophthalmologic emergency requiring immediate specialist intervention.
Clinical Presentation: Symptoms include severe eye pain, significant vision loss, redness, swelling, and sometimes a white or yellow appearance in the pupil. Babies may show extreme irritability, refusing to open the affected eye, and may have fever and signs of systemic illness.
Causes in Infants: Endophthalmitis can result from penetrating eye injuries, spread of infection from other parts of the body through the bloodstream, or rarely as a complication of eye procedures. In newborns, it may develop from infections acquired during birth.
Treatment Urgency: Treatment requires immediate injection of antibiotics directly into the eye, often combined with surgical removal of infected material. Delays of even a few hours can result in complete and permanent vision loss in the affected eye.
Prevention Emergency Eye and Ear Infections in Babies: Any eye injury, sudden vision changes, or severe eye pain requires immediate medical evaluation. Parents should never dismiss sudden changes in an infant’s visual behavior or appearance of the eye.
#3 Mastoiditis: Hearing-Threatening Emergency Ear Infection
Mastoiditis represents a severe complication of ear infections and is classified among the most urgent Emergency Eye and Ear Infections in Babies because it can lead to hearing loss, facial paralysis, or even brain infections.
Progression from Otitis Media: Mastoiditis typically develops as a complication of acute otitis media when infection spreads from the middle ear to the mastoid air cells in the bone behind the ear. The condition is more common in children under 2 years old due to their immature immune systems and anatomical factors.
Recognizing Mastoiditis: Key signs include swelling, redness, and tenderness behind the ear, with the ear appearing to stick out from the head. Children may have fever, irritability, hearing loss, and discharge from the ear. The area behind the ear may feel warm and appear inflamed.
Serious Complications: Untreated mastoiditis can lead to hearing loss, facial nerve paralysis, brain abscess, meningitis, and potentially fatal complications. The infection can spread along bone and soft tissue planes to reach critical structures in the head and neck.
Emergency Treatment: Mastoiditis requires immediate hospitalization with intravenous antibiotics and often surgical drainage of the infected mastoid bone. Early treatment is crucial for preventing permanent hearing loss and life-threatening complications.

#4 Acute Otitis Media: Complicated Emergency Ear Infection
While most ear infections in children are relatively benign, certain presentations of acute otitis media can quickly progress to serious hearing loss in infant complications that requiring emergency intervention.
Suppurative Complications: These include tympanic membrane perforation with persistent drainage, formation of abscesses in the ear canal or surrounding tissues, and spread of infection to adjacent structures. Children may show severe pain, high fever, and systemic signs of illness.
Intracranial Complications: Rare but serious complications include brain abscess, meningitis, and venous sinus thrombosis. Warning signs include severe headache, altered mental status, seizures, focal neurological deficits, and signs of increased intracranial pressure.
Facial Nerve Paralysis: Infection can compress or damage the facial nerve as it passes through the middle ear, causing facial weakness or paralysis. This complication requires immediate medical attention to prevent permanent nerve damage.
Treatment Considerations: Complicated ear infections often require hospitalization, intravenous antibiotics, and sometimes surgical intervention to drain infected material and relieve pressure on vital structures.
Learn more: The Diagnosis and Management of Acute Otitis Media – AAP (American Academy of Pediatrics)
Preseptal vs. Orbital Cellulitis: Critical Differentiation.
Distinguishing between preseptal cellulitis (infection of tissues in front of the orbital septum) and orbital cellulitis (infection behind the septum) is crucial because treatments and outcomes differ dramatically.
Preseptal Cellulitis: This involves infection of the eyelid and surrounding skin but doesn’t affect deeper orbital structures. While concerning, it typically responds well to oral antibiotics and doesn’t threaten vision or life.
Orbital Cellulitis Indicators: Signs that suggest orbital rather than preseptal involvement include restriction of eye movement, pain with eye movement, double vision, decreased vision, and proptosis (eye bulging forward). These findings indicate deeper infection requiring immediate emergency care.
Imaging Requirements: CT scanning is often necessary to distinguish between these conditions and assess the extent of infection. This imaging helps guide treatment decisions and identify complications like abscess formation.
Treatment Differences: Preseptal cellulitis may be treated with oral antibiotics on an outpatient basis, while orbital cellulitis requires immediate hospitalization with intravenous antibiotics and close monitoring for complications.
#5 Neonatal Conjunctivitis: Newborn Emergency Eye Infection
Conjunctivitis in newborns can be caused by various pathogens acquired during birth, some of which can cause permanent vision loss if not treated immediately.
Gonococcal Conjunctivitis: This bacterial infection can cause rapid corneal perforation and permanent vision loss within 24-48 hours if not treated with immediate systemic antibiotics. The condition presents with severe purulent discharge and significant eyelid swelling.
Chlamydial Conjunctivitis: While typically less acute than gonococcal infection, chlamydial conjunctivitis can cause chronic inflammation and scarring if not properly treated. It may also be associated with pneumonia in newborns.
Chemical Conjunctivitis: Caused by prophylactic eye drops given at birth, this condition is typically mild and self-limiting but must be distinguished from infectious causes.
Treatment Protocols: Newborn conjunctivitis requires immediate evaluation and often systemic antibiotic treatment, especially when bacterial causes are suspected. Topical antibiotics alone are insufficient for serious bacterial infections.
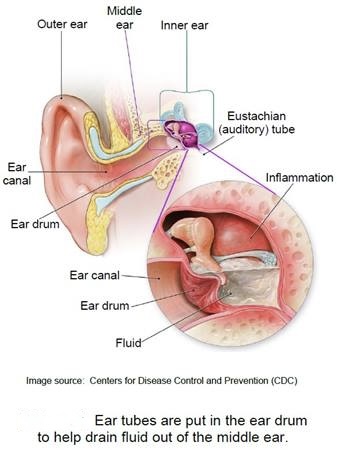
Chronic Otitis Media with Effusion: The Silent Hearing Threat
While not typically an emergency condition, chronic fluid accumulation in the middle ear can cause significant hearing loss during critical periods of speech and language development.
Hearing Loss Impact: Persistent fluid in the middle ear causes conductive hearing loss that can interfere with normal speech and language development, particularly if it occurs during the first years of life when language skills are rapidly developing.
Recognition Challenges: Unlike acute ear infections, chronic effusion often causes minimal pain, making it difficult for parents to recognize. Children may show delayed speech development, behavioral problems, or academic difficulties.
Treatment Considerations: Chronic effusion may require surgical intervention with tympanostomy tube placement to restore normal hearing and prevent developmental delays.
Monitoring Requirements: Children with chronic ear problems require regular hearing assessments and developmental monitoring to ensure normal progress in speech and language skills.
When to Seek Immediate Medical Care for Infant Eye or Ear Problems
Immediate Emergency Signs: Call 911 (in USA) or go to the emergency room immediately for sudden vision loss, severe eye pain with vision changes, signs of orbital cellulitis, suspected endophthalmitis, or any signs of intracranial complications from ear infections.
Urgent Medical Attention: Seek prompt medical care for persistent ear drainage, signs of mastoiditis, facial paralysis, severe headache with ear infection, or any rapid worsening of eye or ear symptoms.
Same-Day Evaluation: Contact your pediatrician immediately for newborn conjunctivitis, eye injuries, sudden hearing loss, or any concerning changes in your child’s vision or hearing.
How to Prevent These 5 Emergency Eye and Ear Infections in Babies
Infection Prevention: Maintain good hygiene, avoid touching eyes with unwashed hands, and seek prompt treatment for upper respiratory infections that could spread to eyes or ears.
Vaccination Benefits: Stay current with recommended vaccinations, including pneumococcal and Haemophilus influenzae vaccines, which can prevent many serious ear and eye infections.
Environmental Factors: Avoid exposure to cigarette smoke, which increases the risk of ear infections, and protect children from eye injuries during play and activities.
Regular Monitoring: Establish regular pediatric care relationships and don’t hesitate to seek evaluation for concerning eye or ear symptoms.
Understanding these 5 emergency eye and ear infections in babies can mean the difference between swift recovery and permanent complications.
Treatment Approaches and Recovery Timelines for Eye and Ear Infections in Babies
Understanding treatment protocols and expected recovery timelines helps parents navigate the challenging experience of managing eye and ear infections in babies while knowing what to expect during healing processes.
Emergency Treatment Protocols for Severe Eye and Ear Infections in Babies
When babies present with emergency eye and ear infections requiring immediate intervention, treatment typically follows aggressive protocols designed to prevent permanent damage while addressing active infections.
Intravenous Antibiotic Therapy: Severe eye and ear infections in babies like orbital cellulitis, endophthalmitis, and mastoiditis require hospitalization with intravenous antibiotics. These infections demand immediate high-dose antibiotics delivered directly into the bloodstream to achieve therapeutic levels quickly enough to prevent permanent damage.
Treatment typically continues for 48-72 hours intravenously before transitioning to oral antibiotics if clinical improvement occurs. Total antibiotic duration often extends 10-14 days to ensure complete eradication of infection and prevent recurrence or complications.
Surgical Interventions: Some eye and ear infections in babies require surgical drainage or decompression procedures. Mastoiditis may need mastoidectomy to remove infected bone. Orbital abscesses require surgical drainage. Endophthalmitis necessitates vitreous tap and injection of antibiotics directly into the eye.
These procedures, while serious, can save vision and hearing when performed promptly. Recovery from surgical interventions typically requires several weeks of careful monitoring and may include restrictions on activities that could stress healing tissues.
Monitoring Requirements: Babies hospitalized for emergency eye and ear infections need frequent assessments including visual acuity testing (when possible), ophthalmologic examinations, hearing evaluations, and neurological monitoring for signs of intracranial complications. Parents should expect multiple daily examinations during acute treatment phases.
Outpatient Treatment for Non-Emergency Eye and Ear Infections in Babies
While not all eye and ear infections in babies require hospitalization, even outpatient cases demand careful attention to treatment protocols and follow-up to ensure complete resolution without complications.
Oral Antibiotic Regimens: Simple bacterial eye and ear infections in babies typically respond to oral antibiotics prescribed for 7-10 days. Common medications include amoxicillin, amoxicillin-clavulanate, or cephalosporins depending on suspected pathogens and local resistance patterns.
Parents must complete the full antibiotic course even if symptoms improve after a few days. Premature discontinuation allows surviving bacteria to multiply, potentially creating antibiotic-resistant strains that make future eye and ear infections in babies harder to treat.
Topical Medications for Eye Infections: Bacterial conjunctivitis and other superficial eye infections may respond to antibiotic eye drops or ointments. Parents must learn proper administration techniques ensuring medications reach infected tissues. Gentle cleaning of discharge before applying medications improves effectiveness.
Viral conjunctivitis requires supportive care only, as antibiotics don’t treat viral infections. However, distinguishing bacterial from viral eye infections requires professional evaluation, so never assume eye discharge is viral without medical confirmation.
Pain Management Strategies: Eye and ear infections in babies cause significant discomfort that interferes with eating and sleeping. Age-appropriate doses of acetaminophen or ibuprofen help manage pain and reduce fever. Warm compresses can soothe affected areas but should not replace medical treatment.
Recovery Timeline Expectations for Eye and Ear Infections in Babies
Parents navigating treatment of eye and ear infections in babies benefit from understanding typical recovery patterns and knowing when slower-than-expected improvement warrants additional medical evaluation.
Acute Symptom Resolution: Most bacterial eye and ear infections in babies show improvement within 48-72 hours of starting appropriate antibiotics. Fever typically resolves within 1-2 days. Eye discharge or ear drainage decreases noticeably. Pain and irritability improve as inflammation subsides.
However, complete resolution takes longer. Eye redness may persist for 1-2 weeks. Middle ear fluid from ear infections can persist for months after acute infection resolves. Parents should maintain realistic expectations about healing timelines.
Hearing Recovery After Ear Infections: Fluid accumulation in middle ears commonly persists for weeks to months after ear infection treatment completes. This causes temporary conductive hearing loss that typically resolves as fluid gradually drains. However, persistent fluid beyond 3 months may require ENT specialist evaluation and possible tube placement.
Parents should monitor speech development carefully after eye and ear infections in babies affecting hearing, as prolonged hearing impairment during critical language development periods can impact communication skills.
Vision Recovery After Eye Infections: Most superficial eye infections resolve completely without lasting vision impact. However, severe infections like endophthalmitis or complications from orbital cellulitis may cause permanent vision changes. Regular follow-up ophthalmology examinations help identify any lasting visual deficits requiring intervention.
Long-Term Monitoring After Serious Eye and Ear Infections in Babies
Babies who survive serious eye and ear infections need ongoing monitoring to identify and address potential long-term complications affecting sensory development and overall health.
Hearing Assessment Schedules: Children with history of serious ear infections or mastoiditis require regular hearing evaluations to ensure normal auditory function. Early detection of hearing loss allows prompt intervention with hearing aids or other technologies supporting normal language development.
Ophthalmologic Follow-Up: Babies who experience orbital cellulitis, endophthalmitis, or other serious eye and ear infections need periodic vision screening to identify problems like amblyopia (lazy eye) developing from unequal vision between eyes. Early detection of vision problems during critical visual development periods allows effective treatment.
Developmental Monitoring: Any sensory impairment from eye and ear infections in babies can affect overall development. Regular developmental screening helps identify delays in speech, language, motor skills, or social development that may relate to visual or hearing deficits. Early intervention services address delays before they significantly impact long-term outcomes.
Preventing Recurrent Eye and Ear Infections in Babies
Babies who experience one episode of eye and ear infections face increased risk for recurrence. Understanding prevention strategies helps break this cycle and protect developing sensory systems.
Prophylactic Interventions: Children with recurrent ear infections may benefit from prophylactic antibiotics or surgical tube placement preventing future episodes. While controversial, these interventions can reduce infection frequency and protect hearing during critical developmental periods.
Environmental Modifications: Eliminating smoke exposure, minimizing daycare attendance during peak respiratory virus season, maintaining current vaccinations, and ensuring adequate nutrition all help reduce recurrence risk for eye and ear infections in babies.
Immune System Support: Breastfeeding provides antibodies protecting against infections. Adequate sleep, proper nutrition, and minimizing stress support healthy immune function reducing susceptibility to recurrent eye and ear infections in babies.
Preparing for parenthood challenges
CONCLUSION:
Your vigilance as a parent can make the difference between recovery and permanent disability. By understanding the risks, recognizing the signs, and acting fast, you can protect your child from the devastating effects of the 5 Emergency Eye and Ear Infections in Babies covered in this guide.
Read more: 5 Emergency Eye and Ear Infections in Babies: Complete Parent’s GuideLooking for comprehensive guidance on caring for your baby? Our book ‘How to Care for Children: From Birth to Age 2’ combines professional nanny experience with evidence based child development research. Written by Kelly and Peter, this guide provides clear, reliable advice rooted in real world childcare. Available in English, Spanish, and Portuguese on Amazon.
Click the link below your preferred language to get your copy!

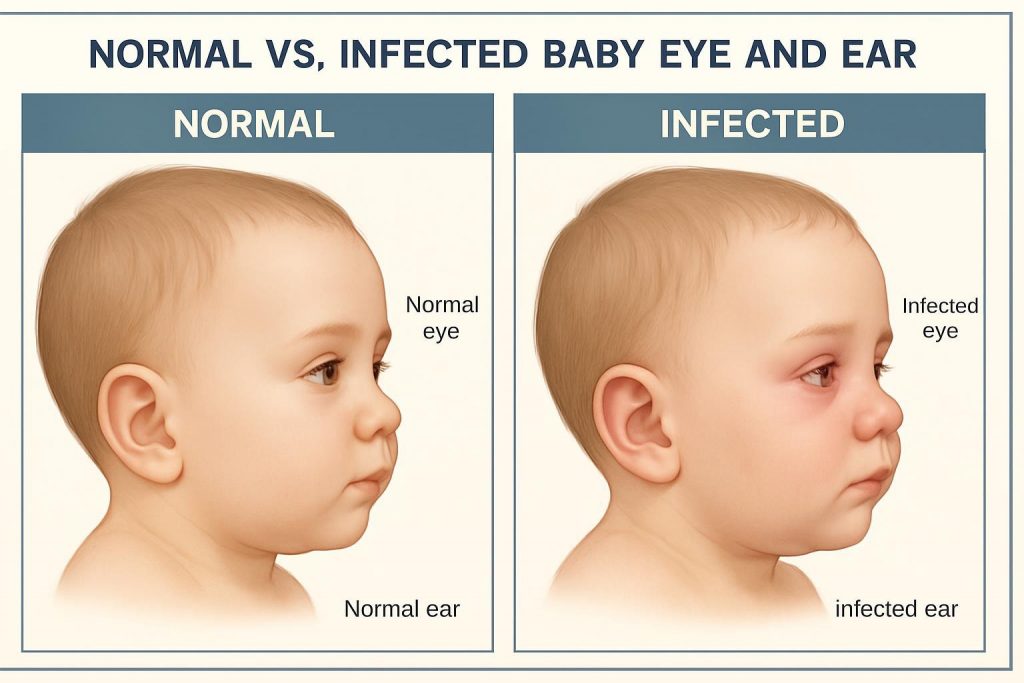
1. How can I tell if my baby has an eye infection?
Look for symptoms such as red or swollen eyes, yellow or green discharge, frequent rubbing, excessive tearing, sensitivity to light, or white/yellow appearance in the pupil.
Emergency signs include severe swelling extending beyond the eyelid, inability to move the eye normally, bulging of the eyeball, sudden vision changes, or high fever with eye symptoms.
Simple conjunctivitis shows mild redness and discharge but allows normal eye movement.
Orbital cellulitis or endophthalmitis cause severe swelling, restricted eye movement, and vision problems requiring immediate emergency care. If you notice concerning signs, consult a pediatrician promptly, and seek emergency care for severe symptoms.
2. What are the warning signs of an ear infection in babies?
Common signs include frequent ear tugging, crying during feeding or lying down, trouble sleeping, fever, fluid draining from the ear, and decreased appetite.
Emergency warning signs include swelling, redness, or tenderness behind the ear (mastoiditis), facial weakness or paralysis, severe headache with ear pain, altered mental status, high fever that doesn’t respond to medication, or rapid symptom progression.
Simple ear infections cause mild discomfort and irritability. Complicated infections like mastoiditis cause visible swelling behind the ear with the ear appearing to stick out from the head. If your baby shows emergency signs, seek immediate medical attention to prevent permanent hearing loss or life-threatening complications.
3. Are eye and ear infections in babies dangerous?
Yes, certain eye and ear infections in babies can be extremely dangerous if left untreated, potentially causing permanent vision loss, hearing loss, or life-threatening complications. Orbital cellulitis can lead to blindness within hours and spread to the brain causing meningitis or brain abscess.
Endophthalmitis can destroy all vision in the affected eye within 6-12 hours. Mastoiditis can cause permanent hearing loss, facial paralysis, meningitis, or brain abscess.
Neonatal conjunctivitis from gonococcal infection can perforate the cornea within 24-48 hours. However, most simple eye and ear infections respond well to treatment when caught early.
The key is recognizing which infections are emergencies requiring immediate care versus routine infections that can be treated with standard antibiotics. Early medical attention ensures safe and effective treatment and prevents serious complications.
4. Can I treat my baby’s infection at home?
No, home remedies are not recommended for eye and ear infections in babies. Only a pediatrician can provide the correct diagnosis and treatment plan, which may include antibiotics, ear drops, or emergency interventions.
Never put breast milk, homeopathic remedies, or over-the-counter drops in your baby’s eyes or ears without medical guidance. Emergency eye and ear infections require immediate professional treatment as delays can cause permanent damage.
Simple infections need proper antibiotics prescribed by a doctor. Even minor-appearing infections can mask serious conditions. Call your pediatrician for any eye discharge, ear drainage, persistent crying, fever, or concerning symptoms.
Seek emergency care immediately for severe swelling, vision changes, inability to move the eye, swelling behind the ear, facial weakness, or rapid symptom progression.
Proper medical care prevents complications and ensures the best outcomes for your baby’s vision and hearing.
5. How can I prevent eye and ear infections in my baby?
Good hygiene is essential. Wash your hands thoroughly before touching your baby’s face or handling feeding equipment. Keep feeding bottles, pacifiers, and toys clean through proper sterilization. Avoid exposure to cigarette smoke, which significantly increases ear infection risk.
Ensure your baby receives all recommended vaccinations, including pneumococcal and Haemophilus influenzae vaccines that prevent many serious ear and eye infections. For newborns, proper eye prophylaxis at birth prevents neonatal conjunctivitis.
Breastfeeding provides antibodies that help prevent infections. Avoid close contact with people who have colds or infections. Never share towels, washcloths, or eye drops between family members. Treat upper respiratory infections promptly to prevent spread to ears.
Keep your baby’s environment smoke-free and minimize daycare exposure when possible. Regular pediatric checkups allow early detection of problems. If infections do occur, complete the full course of prescribed antibiotics even if symptoms improve to prevent antibiotic resistance and recurrence.
Share this life-saving information with other parents and Friends!
Want a complete baby care guide?
Get our FREE checklist sent directly to your inbox - covering everything from birth to age 2, including daily routines, safety guidelines, and developmental milestones.
- ✅ Birth to 3 months essentials
- ✅ 4-12 months routines & alerts
- ✅ 1-2 years development & safety
Enter your email to receive instant access to the PDF