Silent choking in babies present a unique emergency situation that catches many parents completely off-guard. This comprehensive guide will equip you with the essential knowledge to identify, respond to, and prevent these life-threatening situations that affect thousands of infants each year.
When it comes to silent choking in babies, every second counts, and recognizing the warning signs can mean the difference between life and death. Unlike the dramatic choking scenes we see in movies, silent choking in infants is a terrifying reality that occurs without the telltale coughing or crying sounds parents expect to hear.
Age-Specific Choking Risks and Prevention
Newborns to 6 Months
During this stage, babies are not yet eating solid foods, but silent choking babies risks still exist. Common hazards include:
- Small objects left within reach during tummy time
- Loose bedding or stuffed animals in sleep areas
- Sibling’s toys accidentally dropped near baby
- Pacifier parts that become detached
- Small clothing accessories like buttons
Prevention strategies: Keep the baby’s environment completely clear of small objects. Regularly inspect pacifiers and bottle nipples for wear. Never leave baby unattended with older siblings who might share inappropriate toys.
6 to 12 Months
This is when infant airway obstruction risks dramatically increase as babies begin exploring solid foods and have increased mobility.
High-risk foods at this age:
- Chunks of meat or cheese (must be cut into tiny pieces)
- Whole berries (quarter grapes, halve blueberries)
- Crackers or cookies that break into large pieces
- Sticky foods like peanut butter (thin layer only)
- Raw vegetables
Baby-led weaning safety: If practicing baby-led weaning, ensure foods are soft enough to squish between your fingers and cut into appropriate stick shapes that baby can grasp but are too large to fully fit in mouth.
12 to 24 Months
Toddlers face unique baby choking signs risks due to increased independence and desire to feed themselves.
Common hazards:
- Running or playing while eating
- Lying down during meals
- Eating in car seats during travel
- Accessing older siblings’ snacks
- Trying to eat too quickly
Prevention focus: Establish strict mealtime rules: sitting down only, no talking with mouth full, taking small bites, and always supervised by an adult.
Read more: 7 Silent Choking in Babies Signs Every Parent Must KnowAAP Safe Sleep Guidelines – Discussing Overall Baby Safety
What Is Silent Choking in Babies?

Silent choking babies experience complete airway obstruction, preventing them from making any sound whatsoever. Unlike partial choking where babies might cough, cry, or make noise, silent choking creates a medical emergency where the infant cannot breathe, speak, or cry for help.
This infant airway obstruction occurs when food, toys, or other objects completely block the baby’s trachea (windpipe). The silence is what makes this condition so dangerous parents may not immediately realize their child is in distress because there are no obvious audible warning signs.
The Science Behind Silent Choking
When baby choking signs involve complete obstruction, the vocal cords cannot vibrate to produce sound. The baby’s natural reflexes to cough or cry are rendered ineffective, creating a silent emergency that requires immediate intervention.
7 Critical Silent Choking Babies Warning Signs
How to Identify Silent Choking in Babies
1. The Universal Choking Sign
Babies old enough may instinctively grab their throat with both hands. This baby safety emergency signal is often the first visible indication that something is seriously wrong.
2. Inability to Cry or Make Sounds
A baby who was recently making noise but suddenly becomes silent while eating or playing may be experiencing silent choking babies symptoms. The absence of crying during apparent distress is a major red flag.
3. Blue or Purple Skin Color (Cyanosis)
Watch for cyanosis around the lips, face, and fingernails. This infant airway obstruction symptom indicates oxygen deprivation and requires immediate action.
4. Panicked Facial Expression
The baby’s eyes may appear wide and frightened, with a look of panic or terror. This expression often accompanies baby choking signs and indicates the infant’s awareness of their inability to breathe.
5. Weak or Absent Cough
While typical choking involves forceful coughing, silent choking babies may produce only weak coughing sounds or no cough at all, despite obvious signs of distress.
6. Loss of Consciousness
If the baby safety emergency continues without intervention, the infant may become unconscious due to lack of oxygen. This is a critical stage requiring immediate professional medical assistance.
7. Difficulty Swallowing or Drooling
Excessive drooling or apparent difficulty swallowing, especially during mealtime, can indicate infant airway obstruction and potential choking risks.
Tip: Babies under 1 year are especially at risk because they explore with their mouths and have small airways.
Immediate Response to Silent Choking Babies
Read more: 7 Silent Choking in Babies Signs Every Parent Must KnowAmerican Red Cross Infant CPR Course
For Infants Under 12 Months
Step 1: Assess the Situation Quickly determine if the baby is experiencing silent choking babies symptoms by checking for the warning signs listed above.
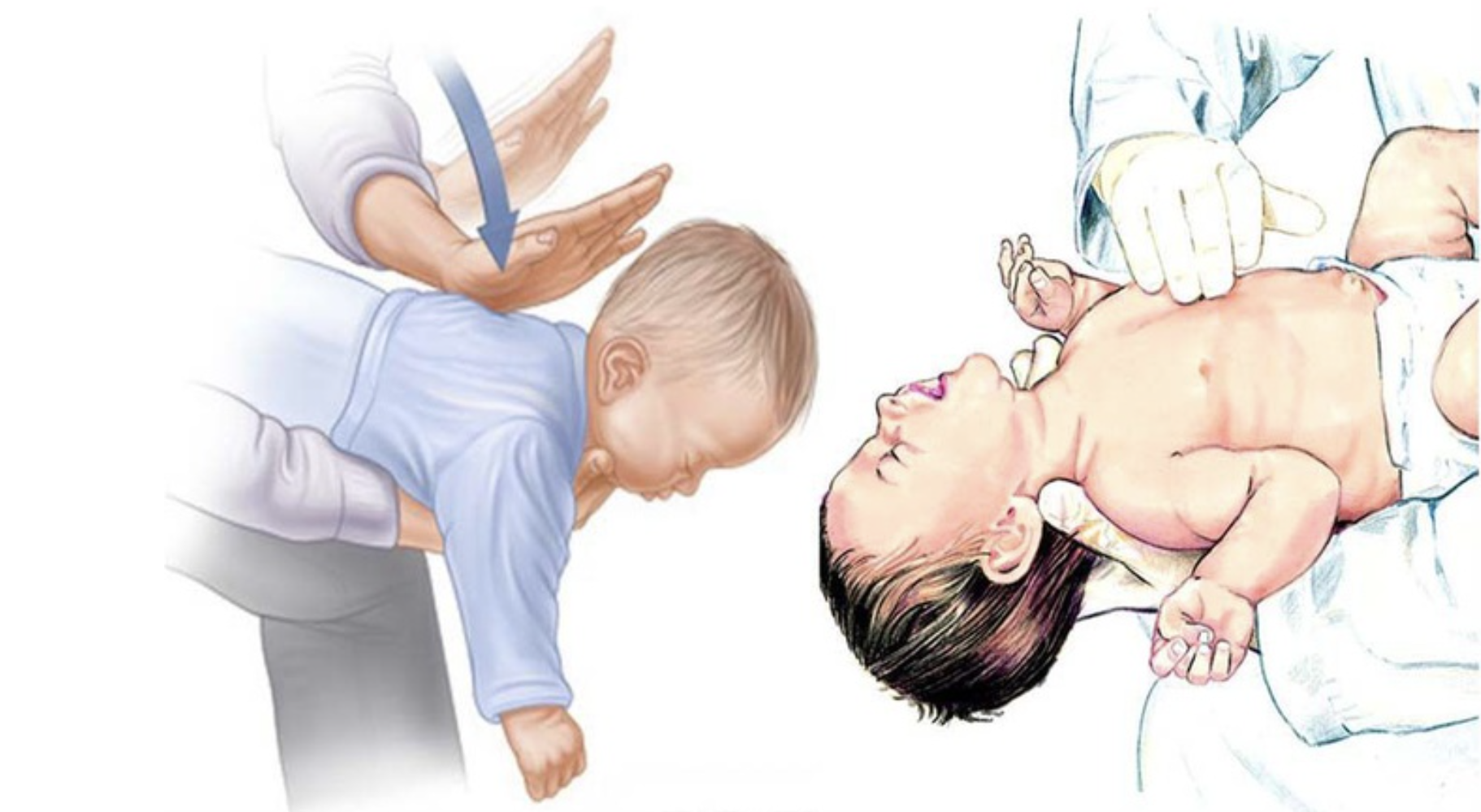
Step 2: Position the Baby Place the infant face-down along your forearm, supporting their head and neck. Ensure the baby’s head is lower than their chest to utilize gravity.
Step 3: Deliver Back Blows Using the heel of your hand, deliver five sharp blows between the baby’s shoulder blades. These back blows help dislodge the obstruction causing baby choking signs.
Step 4: Check the Mouth Look inside the baby’s mouth for visible objects. If you can see something, try to remove it with your finger. Never perform blind finger sweeps, as this can push the obstruction deeper.
Step 5: Chest Thrusts If back blows don’t work, turn the baby face up and perform five chest thrusts using two fingers placed just below the nipple line.
When to Call Emergency Services
Call 911 immediately if:
- The baby becomes unconscious
- Silent choking babies symptoms persist after initial intervention
- You cannot dislodge the obstruction within 30 seconds
- The infant shows signs of severe infant airway obstruction
Prevention Strategies for Baby Safety Emergency
Age-Appropriate Food Guidelines
Understanding which foods pose choking prevention babies risks is crucial:
High Risk Foods to Avoid:
- Whole grapes (cut into quarters)
- Nuts and seeds
- Hard candies
- Popcorn
- Raw vegetables (carrots, celery)
- Hot dogs (cut lengthwise and into small pieces)
Creating a Safe Environment
Baby Proofing for Choking Prevention:
- Remove small objects that pose baby safety emergency risks
- Regularly inspect toys for loose parts
- Keep older children’s toys away from babies
- Maintain clean floors free of small debris
Common Mistakes Parents Make
Mistake 1: Assuming All “Baby Food” Is Safe
Many foods marketed for babies still pose choking prevention babies risks. Even puréed foods can be dangerous if baby takes too large a mouthful or isn’t sitting upright properly.
Solution: Always test food texture yourself. If it doesn’t easily dissolve or can’t be mashed against the roof of your mouth, it’s not appropriate for your baby’s developmental stage.
Mistake 2: Not Knowing CPR
Many parents delay learning infant CPR, thinking they’ll “take the class eventually.” In a baby safety emergency, every second counts, and there’s no time to Google instructions.
Solution: Take an infant CPR certification course before your baby starts solid foods. Refresh this training annually as recommendations can change.
Mistake 3: Relaxing Supervision Around Experienced Eaters
Parents often become less vigilant once babies seem comfortable with eating, but choking can happen to any child at any meal.
Solution: Maintain the same level of supervision regardless of your baby’s eating experience. Never leave room during mealtime, even “just for a second.”
Mistake 4: Giving Food to Keep Baby Quiet
Using snacks to occupy babies during car rides, shopping, or other activities when you can’t provide full attention creates significant infant airway obstruction risks.
Solution: Only offer food when you can provide complete supervision. Plan activities around meal and snack times rather than using food as a convenience tool.
Mistake 5: Following Older Parenting Advice
Grandparents and older relatives may suggest foods or practices that were common decades ago but are now known to be dangerous.
Solution: Politely educate family members on current safety guidelines. Provide them with written information on safe foods and choking prevention babies strategies.
After a Choking Incident: What Comes Next
Immediate Medical Evaluation
Even if you successfully dislodge an obstruction and your baby appears fine, medical evaluation is crucial. Silent choking babies may have suffered:
- Minor airway injuries
- Lingering partial obstructions
- Inflammation from the incident
- Psychological trauma requiring monitoring
When to seek immediate emergency care:
- Baby lost consciousness during incident
- You’re unsure if obstruction was completely cleared
- Baby has difficulty breathing after incident
- Unusual behavior or lethargy following choking
- Any signs of respiratory distress
Psychological Recovery for Parents
Witnessing baby choking signs and experiencing a baby safety emergency is traumatic for caregivers. It’s normal to experience:
- Heightened anxiety around mealtimes
- Difficulty sleeping
- Replaying the incident mentally
- Excessive worry about future choking
Healthy coping strategies:
- Talk about the experience with supportive friends or family
- Consider short-term counseling if anxiety persists
- Join parent support groups to process feelings
- Review what you did right to boost confidence
- Update your emergency preparedness to feel more in control
Rebuilding Confidence in Feeding
After a choking scare, parents often struggle with feeding anxiety. Some may revert to only offering purées, potentially delaying oral motor skill development.
Gradual reintroduction:
- Start with foods you feel most comfortable offering
- Keep portions very small initially
- Ensure baby is in optimal position (upright, calm, alert)
- Watch for your own anxiety cues that might stress baby
- Celebrate successful meals without incident
Teaching Older Babies About Safety
As babies approach toddlerhood, you can begin introducing age-appropriate safety concepts:
- Simple rules: “Food stays at the table”
- Modeling: Showing careful chewing
- Practice: Encouraging small bites
- Praise: Acknowledging safe eating behavior
Proper Feeding Techniques
Safe Feeding Practices:
- Always supervise mealtime
- Ensure babies are sitting upright while eating
- Introduce new foods gradually
- Cut food into appropriate sizes (no larger than 1/2 inch)
Toddler Safety: Essential Tips to Keep Your Child Safe and Secure
What to Do? First Aid for Silent Choking in Babies
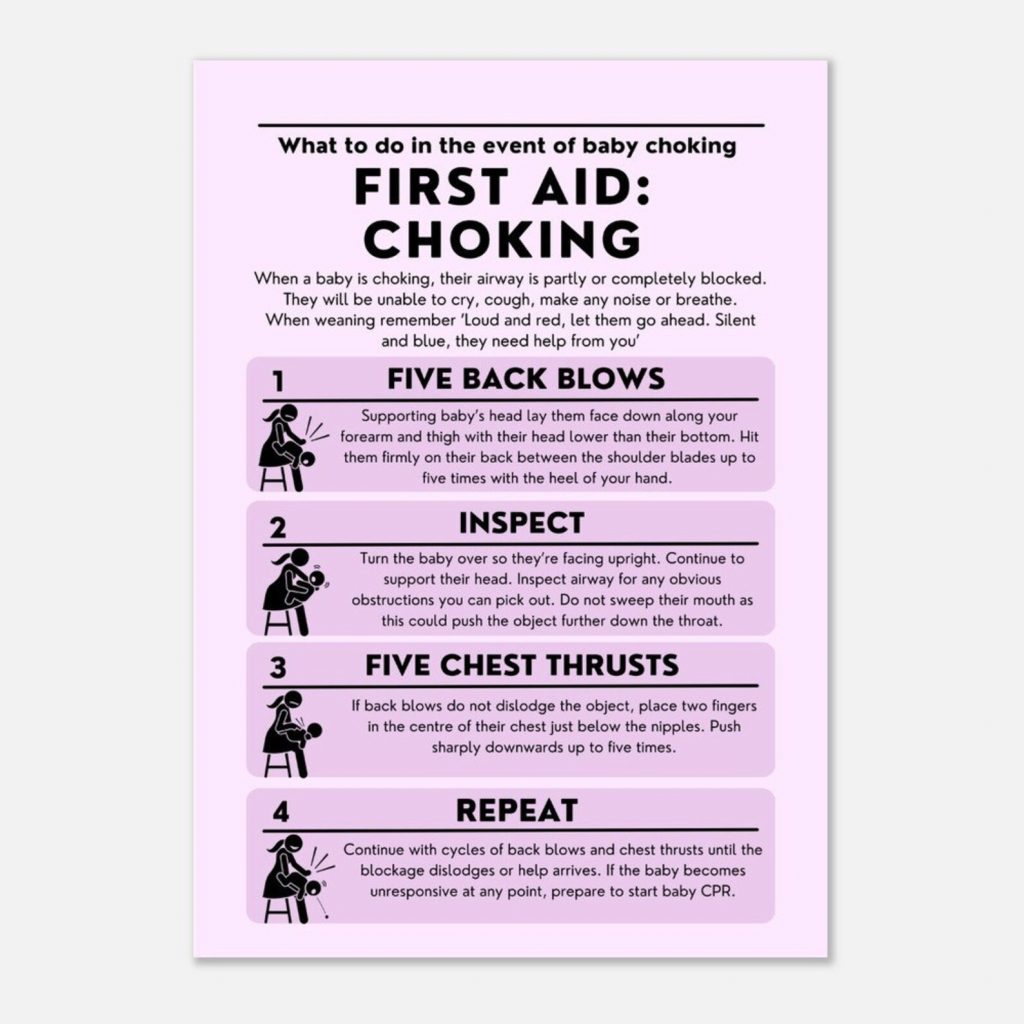
Credit of this image: Etsy.com
If you suspect silent choking in a baby:
- Stay calm but act immediately.
- Call emergency services
- For babies under 1 year:
- Place baby face down on your forearm, supporting head and neck.
- Deliver 5 firm back blows between the shoulder blades.
- Turn the baby face up and perform 5 chest thrusts using two fingers in the center of the chest.
- Repeat until the object is expelled or help arrives.
Never perform the Heimlich maneuver on babies under 1 year old.
Prevention: How to Avoid Silent Choking in Babies
- Cut food into pea-sized pieces
- Avoid hard, sticky, or small round foods
- Keep floors and play areas free from small objects
- Supervise meal and playtime
- Learn infant first aid
Even if the object is expelled, take your baby to the doctor to check for airway injury or lingering blockages.

Final Thoughts on Silent Choking in Babies
Understanding silent choking in babies and learning how to react can make the difference between life and death. Prevention, vigilance, and first aid knowledge empower parents to protect their little ones.
Read more: 7 Silent Choking in Babies Signs Every Parent Must KnowNational Safety Council Choking Prevention
7 Alarming Ways Pacifier Harm Baby Development Long-Term
Looking for comprehensive guidance on caring for your baby? Our book ‘How to Care for Children: From Birth to Age 2’ combines professional nanny experience with evidence based child development research. Written by Kelly and Peter, this guide provides clear, reliable advice rooted in real world childcare. Available in English, Spanish, and Portuguese on Amazon.
Click the link below your preferred language to get your copy!

1. What is the difference between regular choking and silent choking in babies?
Regular choking involves partial airway obstruction where babies can still cough, cry, or make sounds as they try to clear the blockage. Silent choking occurs when the airway is completely blocked, preventing any sound production. The baby cannot cough, cry, or breathe, making it a true medical emergency requiring immediate intervention. Silent choking is more dangerous because parents may not immediately realize their baby is in distress due to the absence of audible warning signs.
2. What are the most common causes of silent choking in babies?
The most common causes include: whole grapes or cherry tomatoes, chunks of meat or cheese, hard candies, nuts and seeds, popcorn, raw vegetables like carrots, hot dogs cut into rounds, and large pieces of soft foods like bananas. Non-food items like small toy parts, coins, buttons, and balloons also frequently cause choking. Babies under 12 months are especially vulnerable because they explore everything with their mouths and have small airways.
3. How quickly must I act if I suspect silent choking?
You must act within seconds. Brain damage from oxygen deprivation can begin within 4-6 minutes. If you notice silent choking signs like inability to cry, blue skin color, panicked expression, or loss of consciousness, immediately begin back blows and chest thrusts while someone calls 911. Do not wait to see if the baby will cough it up on their own, complete airway obstruction requires immediate intervention.
4. Can I perform the Heimlich maneuver on a baby?
No, never perform the Heimlich maneuver on babies under 12 months old. Their internal organs are too delicate and the technique can cause serious injury. Instead, use the infant choking protocol: 5 back blows between shoulder blades with baby face-down on your forearm, then 5 chest thrusts with baby face-up. Alternate between these techniques until the object is expelled or emergency services arrive.
5. What should I do immediately after successfully clearing a choking obstruction?
Even if your baby appears fine after you clear the obstruction, seek immediate medical evaluation. Silent choking can cause hidden injuries like airway inflammation, minor tears, or lingering partial obstructions. Additionally, medical professionals need to ensure no fragments remain in the airway and check for any complications. Always err on the side of caution with baby safety emergencies.
6. How can I practice infant choking first aid without a real emergency?
Take a certified infant CPR and choking relief course through organizations like the American Red Cross, American Heart Association, or local hospitals. These courses use infant mannequins to practice proper technique. Many courses offer both in-person and online options. Practice regularly (every 6-12 months) to maintain muscle memory. Never practice choking relief techniques on a real baby as this could cause injury.
7. At what age do babies become less susceptible to choking?
Choking remains a significant risk throughout childhood, but risk decreases as children develop better chewing skills, understand safety rules, and have larger airways. The highest risk period is 6 months to 3 years old. However, children under 5 years should still avoid high-risk foods like whole grapes, hard candies, and popcorn. Supervision during meals remains important through preschool years and beyond.
8. Should I cut all foods into specific sizes to prevent choking?
Yes, for babies 6-12 months, cut foods into pieces no larger than 1/2 inch. For round foods like grapes and cherry tomatoes, quarter them lengthwise. For foods like hot dogs, slice lengthwise into strips, then cut into small pieces. Avoid giving hard, sticky, or slippery foods that can lodge in the airway. As babies develop better eating skills around 12-18 months, you can gradually introduce slightly larger pieces while maintaining close supervision.



Que legal!
Parabéns!
Tudo relacionado a bebês é muito importante as informações.
Muito obrigada.
Um abraço,
Thank you!
Parabéns!
Que legal!
Toda a informação a respeito de bebês é muito importante.
Muito obrigada.
Estarei sempre colocando mais posts. Espero que gostes também.
Fico feliz que tenhas gostado.
Um abraço.
Muito obrigada por ter dado uma olhada e comentar.
Deixe-me saber se você quer saber de algo que eu não tenha postado ainda, ok?
Um abraço,
Thank you!
This information is extremely helpful.
I will continue to follow your blog!
Thank you!
Really helpful and actionable advice here. Sharing this with new parents I know—this information could actually save a baby’s life.”
Thank you!