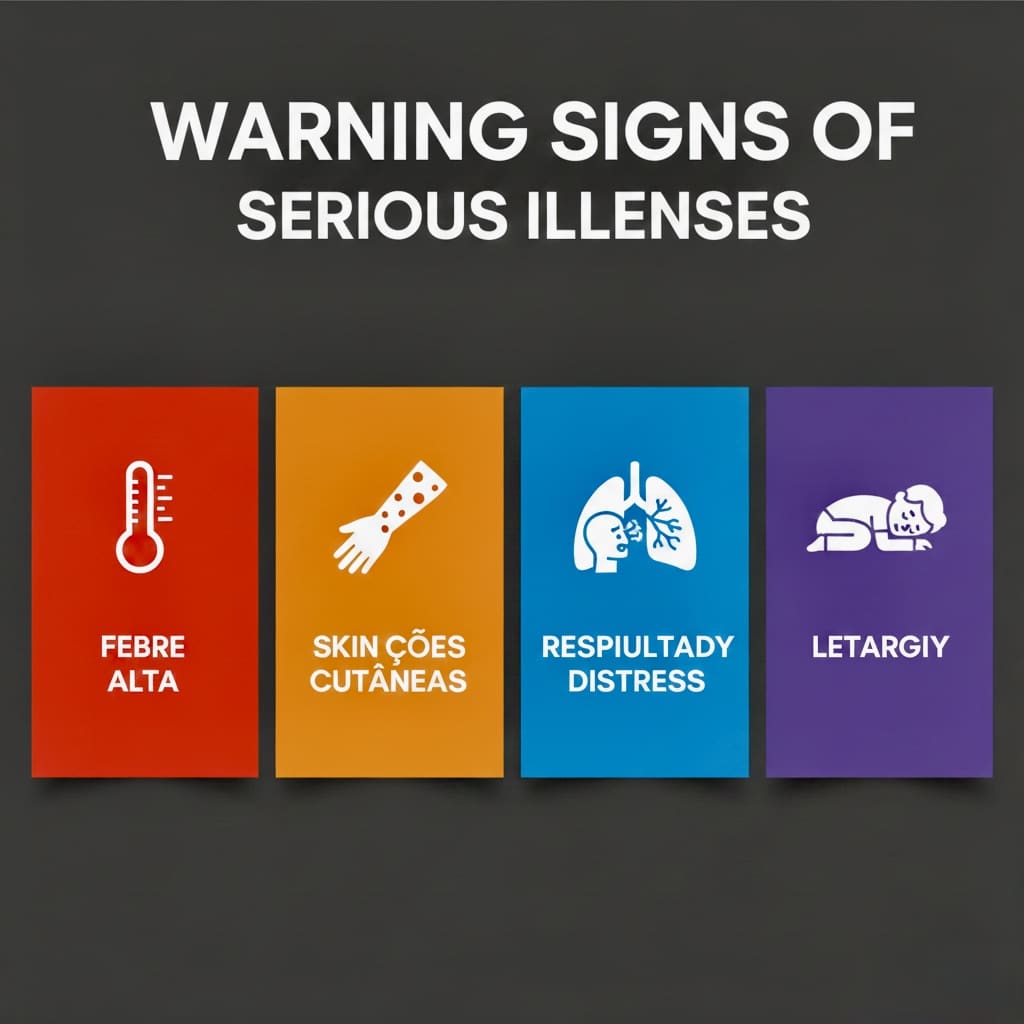
Discover the 7 dangerous toddler illnesses that can escalate from minor symptoms to life-threatening emergencies within hours. This comprehensive guide reveals critical pediatric warning signs, serious childhood diseases symptoms, and exactly when to seek emergency care. Learn how to recognize meningitis, pneumonia, sepsis, and other toddler health emergencies before it’s too late to save your child.
Recognizing dangerous toddler illnesses can save your child’s life. Every parent needs to understand the warning signs of dangerous toddler illnesses before a minor symptom becomes a medical emergency. The toddler years bring a terrifying paradox for parents, your little one is becoming increasingly independent and adventurous, yet they remain utterly vulnerable to serious illnesses that can escalate from seemingly minor symptoms to life-threatening emergencies within hours. Unlike infants who clearly appear unwell, toddlers may continue playing and acting relatively normal even while harboring dangerous infections or conditions that require immediate medical intervention.
Toddler Safety: Essential Tips to Keep Your Child Safe and Secure

Understanding dangerous toddler illnesses is critical because toddlers’ developing immune systems, combined with their natural tendency to explore everything through touch and taste, expose them to health threats. Recognizing the subtle but critical warning signs of serious illness can literally mean the difference between a full recovery and permanent disability or worse.
This essential guide will transform you from an anxious parent into a vigilant health guardian, equipped with the knowledge to identify dangerous conditions before they progress beyond the point of successful treatment.
Understanding Dangerous Toddler Illnesses and Health Vulnerability
Between ages 12 months and 3 years, children face unique health challenges that differ significantly from both infant and older childhood illnesses. Their immune systems are more developed than newborns but still immature compared to school-age children. This creates a dangerous window where toddlers can contract serious infections while lacking the immune response needed to fight them effectively.
The American Academy of Pediatrics emphasizes that toddlers’ natural behavior, putting objects in their mouths, close physical contact with other children, and limited hygiene awareness, significantly increases their exposure to pathogens. Additionally, their small body size means infections can quickly affect vital organs and systems, making rapid recognition and treatment crucial.
This knowledge about dangerous toddler illnesses empowers parents to act quickly when symptoms appear.
Read more: 7 Dangerous Toddler Illnesses Every Parent Must Recognize Before It’s Too Late to Save Their ChildAmerican Academy of Pediatrics Emphasizes Safety and Importance of Vaccines
Meningitis: The Most Life-Threatening Symptom Toddlers Experience
Bacterial meningitis represents one of the most terrifying threats to toddler health because it can progress from mild symptoms to life-threatening complications within 6-12 hours. This infection of the protective membranes surrounding the brain and spinal cord can cause permanent brain damage, hearing loss, or death if not treated immediately.
Recognizing Life-Threatening Symptoms Toddlers Display: High fever combined with severe headache (toddlers may cry inconsolably or hold their heads), stiff neck (child resists having head moved forward), unusual drowsiness or difficulty waking, irritability when touched or moved, nausea and vomiting, and sensitivity to light. A distinctive purple or red rash that doesn’t fade when pressed with a glass indicates blood poisoning and requires immediate emergency care.
The Danger Window: Unlike adults who clearly exhibit severe symptoms, toddlers with meningitis may initially appear to have a simple fever or cold. Parents often wait to see if symptoms improve, but this delay can be fatal. Any combination of fever with unusual behavior changes warrants immediate medical evaluation.
Prevention and Action: Vaccines prevent most common forms of bacterial meningitis, but not all strains. If you suspect meningitis, don’t wait for symptoms to worsen, seek emergency medical care immediately. Treatment with antibiotics must begin within hours to prevent permanent damage.
Meningitis ranks among the most dangerous toddler illnesses because it progresses rapidly from mild symptoms to life-threatening complications.
Read more: 7 Dangerous Toddler Illnesses Every Parent Must Recognize Before It’s Too Late to Save Their ChildEssential Vaccination Schedule to Keep Your Baby Healthy and Protected
Pneumonia is one of the dangerous toddler illnesses that parents often underestimate initially.
Pneumonia: A Serious Childhood Disease Affecting Breathing
Prevention Strategies for Serious Childhood Diseases: Pneumonia in toddlers can be particularly dangerous because their small airways become blocked more easily, and their developing lungs cannot efficiently exchange oxygen. What begins as a cold or cough can rapidly progress to severe breathing difficulties requiring hospitalization.

Recognizing Pneumonia: Fast or labored breathing (more than 40 breaths per minute), chest retractions (skin pulling in around ribs when breathing), persistent cough with thick mucus, high fever, decreased appetite and activity level, and blue coloring around lips or fingernails indicating oxygen deficiency.
Bacterial vs. Viral: Bacterial pneumonia typically develops more rapidly with higher fevers and more severe symptoms, while viral pneumonia may progress more gradually. Both types can be serious in toddlers and require medical evaluation to determine appropriate treatment.
When to Seek Emergency Care: Any signs of breathing difficulty, blue coloring, inability to keep fluids down, or extreme lethargy require immediate medical attention. Pneumonia can quickly progress to respiratory failure in young children.
Kawasaki Disease: Pediatric Warning Signs Parents Miss
Kawasaki disease is a rare but serious condition that causes inflammation of blood vessels throughout the body, potentially leading to heart complications if untreated. It primarily affects children under 5 years old and can be difficult to diagnose because symptoms mimic other common childhood illnesses.
Although rare, Kawasaki disease belongs to the category of dangerous toddler illnesses that require immediate recognition.
Five Key Symptoms: Prolonged fever lasting 5 or more days, red eyes without discharge, swollen lymph nodes in the neck, rash on trunk and genital area, and changes to hands and feet including redness, swelling, and later peeling skin. Additional symptoms may include irritability, sore throat, and swollen tongue with a “strawberry” appearance.
The Treatment Window: Kawasaki disease must be treated within 10 days of fever onset to prevent heart complications. Treatment with intravenous immunoglobulin and aspirin can significantly reduce the risk of coronary artery damage.
Why It’s Overlooked: Many parents and even healthcare providers initially mistake Kawasaki disease for viral infections or other common childhood illnesses. The combination of symptoms, rather than any single symptom, suggests this condition.
Severe Dehydration: Toddler Health Emergency From Common Illnesses
When Toddler Health Emergencies Require Immediate Care: Toddlers can become dangerously dehydrated much faster than adults due to their higher surface area to body weight ratio and faster metabolism. What begins as simple vomiting or diarrhea can quickly become life-threatening if fluid losses aren’t replaced adequately.
Dehydration Warning Signs: Fewer than three wet diapers in 24 hours (for children still in diapers), dark yellow urine with strong odor, dry mouth and sticky saliva, sunken eyes or fontanelle (soft spot), loss of skin elasticity (skin tents when pinched), extreme thirst followed by refusal to drink, and decreased activity or responsiveness.
Severe Dehydration Symptoms: Rapid heartbeat, rapid breathing, sunken eyes, dry mucous membranes, decreased urination, and altered mental state including confusion or extreme irritability. These symptoms require immediate emergency medical care.
Prevention and Management: Offer small, frequent sips of appropriate fluids (breast milk, formula, or oral rehydration solutions for babies; water and appropriate solutions for older toddlers). Avoid giving plain water to children under 12 months, as it can cause dangerous electrolyte imbalances.
Dehydration represents one of the most common yet dangerous toddler illnesses that escalates quickly without proper intervention.
Febrile Seizures: When Dangerous Toddler Illnesses Cause Convulsions
Febrile seizures affect 2-5% of children between 6 months and 5 years old and can be absolutely terrifying for parents to witness. While most febrile seizures are harmless, they can indicate serious underlying infections and require careful evaluation.
Types of Febrile Seizures: Simple febrile seizures last less than 15 minutes, involve the whole body, and don’t recur within 24 hours. Complex febrile seizures last longer than 15 minutes, may be partial (affecting only part of the body), or recur within 24 hours. Complex seizures require more extensive medical evaluation.
Immediate Response: Stay calm, place the child on their side on a safe surface, don’t put anything in their mouth, time the seizure, and call emergency services if the seizure lasts more than 5 minutes or if the child has difficulty breathing afterward.
When to Worry: First-time seizures, seizures in children under 12 months or over 6 years, seizures lasting longer than 15 minutes, or seizures accompanied by serious illness symptoms require immediate medical evaluation.
Febrile seizures, while often benign, can indicate dangerous toddler illnesses requiring medical evaluation.
Sepsis: Critical Life-Threatening Symptoms in Toddlers
Sepsis is among the most rapidly progressing dangerous toddler illnesses, requiring immediate emergency care.
Sepsis occurs when the body’s response to infection damages its own organs and can rapidly progress to septic shock and death. Toddlers are at higher risk because their immune systems may overreact to infections, and symptoms can be subtle initially.
Early Sepsis Signs: High fever or unusual low body temperature, rapid heart rate, rapid breathing, unusual skin color (pale, mottled, or blue), decreased urination, and altered mental state including confusion, extreme sleepiness, or unusual irritability.
Progressive Symptoms: As sepsis worsens, children may develop severe breathing difficulties, very low blood pressure, skin rash or discoloration, and decreased responsiveness. These late-stage symptoms require immediate intensive medical care.
Risk Factors: Recent infections, recent surgery or medical procedures, chronic medical conditions, and compromised immune systems increase sepsis risk. Any child with concerning symptoms after recent illness should be evaluated promptly.
Intussusception: Hidden Pediatric Warning Signs of Intestinal Blockage
Intussusception occurs when part of the intestine slides into an adjacent part, creating a blockage that can cut off blood supply to the affected area. This condition is most common in children between 6 months and 3 years old and requires emergency treatment to prevent intestinal damage.
Classic Symptoms: Sudden onset of severe abdominal pain causing child to draw knees to chest and cry intensely, vomiting that may become bile-colored (green), and “currant jelly” stools containing blood and mucus. Between pain episodes, children may seem relatively normal, which can delay diagnosis.
The Danger of Delay: Intussusception can cause intestinal tissue death within hours if blood supply is compromised. Early treatment with air or contrast enemas can often resolve the condition without surgery, but delays may require surgical intervention.
When to Act: Severe abdominal pain that comes in waves, especially when combined with vomiting or unusual stools, requires immediate medical evaluation. Don’t wait to see if symptoms improve.
Intussusception joins the list of dangerous toddler illnesses that demand swift action to prevent permanent damage.

Emergency Action Plan for Serious Childhood Diseases
Know Your Child’s Baseline: Creating an action plan for dangerous toddler illnesses starts with knowing your child’s baseline health. Understanding dangerous toddler illnesses helps you recognize when something is seriously wrong.
Establish Healthcare Relationships: Develop relationships with your pediatrician and identify the nearest emergency room or urgent care facility. Know which conditions require emergency care versus those that can wait for regular office hours.
Document Symptoms: Keep notes about symptoms including timing, duration, severity, and any associated factors. This information helps healthcare providers make accurate diagnoses and treatment decisions.
Emergency Contacts: Maintain updated lists of emergency contacts including your pediatrician’s after-hours number, poison control center, and local emergency services. Program these numbers into your phone and post them in your home.
The goal isn’t to become paranoid about every sniffle, but to develop expertise in recognizing dangerous toddler illnesses when they occur. Quick recognition of dangerous toddler illnesses can save lives and prevent long-term complications.
15 Amazing Baby Essentials Every Parent Needs in 2025
Looking for comprehensive guidance on caring for your baby? Our book ‘How to Care for Children: From Birth to Age 2’ combines professional nanny experience with evidence based child development research. Written by Kelly and Peter, this guide provides clear, reliable advice rooted in real world childcare. Available in English, Spanish, and Portuguese on Amazon.
Click the link below your preferred language to get your copy!

1. How quickly can dangerous toddler illnesses become life-threatening?
Some dangerous toddler illnesses can progress from mild symptoms to life-threatening emergencies within 6 to 12 hours. Bacterial meningitis represents one of the fastest progressions, potentially causing permanent brain damage or death within hours without treatment.
Sepsis can escalate even more rapidly, with a child appearing mildly ill in the morning and requiring intensive care by afternoon. Dehydration from vomiting or diarrhea can become critical within 24 hours in toddlers due to their small body size. Intussusception requires treatment within hours to prevent intestinal tissue death.
The key is recognizing that toddlers often hide serious illness symptoms by continuing to play or act relatively normal until the condition becomes severe. Parents should never adopt a wait and see approach when multiple warning signs appear together, as this delay can mean the difference between simple treatment and permanent complications.
2. What temperature is considered dangerous for toddlers?
A rectal temperature of 100.4°F (38°C) or higher in children under 3 months requires immediate medical evaluation. For toddlers aged 12 to 36 months, fever becomes concerning when it reaches 102°F (39°C) or higher, lasts more than 24 hours without obvious cause, or accompanies other dangerous symptoms. However, the fever number alone doesn’t tell the complete story.
A toddler with 101°F who appears extremely lethargic, refuses all fluids, has difficulty breathing, or shows signs of confusion needs immediate care regardless of the specific temperature. Some serious childhood diseases like sepsis can actually cause abnormally low body temperature rather than fever.
The concerning factors include how the child looks and acts, whether fever responds to medication, if the child can maintain hydration, and whether other symptoms accompany the temperature elevation. Always trust your instincts when fever combines with unusual behavior changes, as this combination often signals dangerous toddler illnesses requiring prompt medical attention.
3. Should I take my toddler to the emergency room or urgent care?
Emergency rooms handle life-threatening symptoms requiring immediate intervention, while urgent care manages serious but not critical conditions.
Take your toddler to the emergency room for difficulty breathing, blue lips or skin, seizures lasting more than 5 minutes, severe dehydration symptoms, suspected meningitis signs, uncontrollable bleeding, severe allergic reactions, loss of consciousness, extreme lethargy or inability to wake, severe abdominal pain with vomiting, or any combination of symptoms suggesting dangerous toddler illnesses.
Urgent care works well for high fevers without alarming symptoms, minor injuries, ear infections, mild dehydration, coughs and colds needing evaluation, or situations where your pediatrician cannot see your child same day.
When uncertain, call your pediatrician first for guidance, as they know your child’s medical history and can help determine the appropriate care level. Remember that emergency rooms prioritize patients by severity, so your wait time reflects how sick staff perceive your child to be compared to other patients.
4. Can toddlers hide serious illness symptoms?
Yes, toddlers frequently mask serious childhood diseases through continued activity and play until conditions become severe. Young children have remarkable energy reserves that allow them to appear relatively normal even while harboring dangerous infections.
A toddler with early pneumonia might still run around the house despite developing lung infection. Children with meningitis often seem to have simple fever initially before neurological symptoms emerge.
This masking effect occurs because toddlers cannot articulate how they feel, their immune systems respond differently than adults, and their natural drive to play overrides discomfort until illness becomes overwhelming.
Additionally, toddlers lack the reference points to know something feels wrong in their bodies. Parents must look beyond surface behavior to notice subtle changes like decreased appetite, less enthusiasm during favorite activities, unusual clinginess, changes in sleep patterns, or reduced interaction with toys.
The dangerous aspect of this masking is that parents may delay seeking care because the child doesn’t appear very sick, losing critical treatment time for conditions requiring immediate intervention.
5. What should I include in my home first aid kit for toddler emergencies?
Every parent should maintain a comprehensive first aid kit specifically designed for dangerous toddler illnesses and emergencies.
Essential items include a reliable digital thermometer for accurate temperature readings, oral rehydration solution packets for preventing dehydration, children’s acetaminophen and ibuprofen with proper dosing instructions, adhesive bandages in various sizes, sterile gauze pads and medical tape, antibiotic ointment, tweezers for splinter removal.
Children’s antihistamine for allergic reactions, a nasal aspirator, and a current list of emergency contacts including your pediatrician’s after hours number and poison control center. Store medications in child proof containers but where you can access them quickly during emergencies.
Include a small flashlight for checking throat and pupils, and keep written dosing charts based on your child’s current weight since proper medication dosing prevents dangerous errors. Replace expired medications every six months and update emergency contacts annually.
Consider adding a basic first aid manual with pictures showing how to recognize serious childhood diseases symptoms. Keep this kit in an accessible location that all caregivers know about, and maintain a duplicate kit in your vehicle for emergencies away from home.